Affordable Care Act
Together with the Health Care and Education Reconciliation Act of 2010 amendment, it represents the U.S. healthcare system's most significant regulatory overhaul and expansion of coverage since the enactment of Medicare and Medicaid in 1965.
The mandate and limits on open enrollment[49][50] were designed to avoid the insurance death spiral, minimize the free rider problem and prevent the healthcare system from succumbing to adverse selection.
The exchanges are regulated, largely online marketplaces, administered by either federal or state governments, where individuals, families and small businesses can purchase private insurance plans.
The Supreme Court reversed this ruling in the consolidated case, Maine Community Health Options v. United States, reaffirming as with Judge Wheeler that the government had a responsibility to pay those funds under the ACA and the use of riders to de-obligate its from those payments was illegal.
[113] To obtain a waiver, a state must pass legislation setting up an alternative health system that provides insurance at least as comprehensive and as affordable as ACA, covers at least as many residents and does not increase the federal deficit.
The 1993 Republican Health Equity and Access Reform Today (HEART) Act, contained a "universal coverage" requirement with a penalty for noncompliance—an individual mandate—as well as subsidies to be used in state-based 'purchasing groups'.
[141] Orszag had previously been director of the Congressional Budget Office, and under his leadership the agency had focused on using cost analysis to create an affordable and effective approach to health care reform.
Obama proposed private and public group insurance, income-based subsidies, consumer protections, and expansions of Medicaid and SCHIP, which was estimated at the time to reduce the number of uninsured people by 33.9 million by 2018 at a higher cost.
This group—in particular, Democrats Max Baucus, Jeff Bingaman and Kent Conrad, along with Republicans Mike Enzi, Chuck Grassley and Olympia Snowe—met for more than 60 hours, and the principles they discussed, in conjunction with the other committees, became the foundation of a Senate bill.
[157][158][159] Congressional Democrats and health policy experts, such as MIT economics professor Jonathan Gruber[160] and David Cutler, argued that guaranteed issue would require both community rating and an individual mandate to ensure that adverse selection or "free riding" would not result in an insurance "death spiral".
By deliberately drawing on bipartisan ideas—the same basic outline was supported by former Senate Majority Leaders Howard Baker, Bob Dole, Tom Daschle and George J. Mitchell—the bill's drafters hoped to garner the necessary votes.
[227][229] A 2016 DHHS study found that states that expanded Medicaid had lower premiums on exchange policies, because they had fewer low-income enrollees, whose health on average is worse than that of those with higher income.
[235] Another study, using Surveillance, Epidemiology, and End Results (SEER) Program data from 2010 to 2014, found that Medicaid expansion was associated with a 6.4% net increase in early stage (in situ, local, or regional) diagnoses of all cancers combined.
[234] An analysis of Behavioral Risk Factor Surveillance System (BRFSS) survey data found a 2.8% annual increase in viral suppression rates among all PLWH from 2010 to 2015 due to Medicaid expansion.
[243] A July 2019 study by the National Bureau of Economic Research (NBER) indicated that states enacting Medicaid expansion exhibited statistically significant reductions in mortality rates.
Critics argue that Medicaid expansion has not reduced cost-sharing by a significant margin, as the amount households paid out of pocket for healthcare over the past ten years (in the form of deductibles, co-payments, etc.)
For example, the Kaiser Family Foundation reported that for the second-lowest cost "Silver plan", a 40-year old non-smoker making $30,000 per year would pay effectively the same amount in 2017 as they did in 2016 (about $208/month) after the tax credit, despite a large increase in the list price.
[260][clarification needed] Paul Krawzak claimed that even if cost controls succeed in reducing the amount spent on healthcare, such efforts on their own may be insufficient to outweigh the long-term burden placed by demographic changes, particularly the growth of the population on Medicare.
In addition, many employees chose to combine a health savings account with higher deductible plans, making the net impact of ACA difficult to determine precisely.
[239][271] A study of 10,010 women aged 18–26 identified through the 2008-12 National Health Interview Survey found that the likelihood of HPV vaccination initiation and completion increased by 7.7 and 5.8 percentage points respectively when comparing before and after October 1, 2010.
[325][326] Other confounding impacts include that health insurance helps attract and retain employees, increases productivity and reduces absenteeism; and lowers corresponding training and administration costs from a smaller, more stable workforce.
[347] After the Supreme Court upheld the individual mandate, a 2012 poll held that "most Americans (56%) want to see critics of President Obama's health care law drop efforts to block it and move on to other national issues".
[370] IPAB was given the authority to recommend cost-saving changes to Medicare by facilitating the adoption of cost-effective treatments and cost-recovering measures when statutory expenditure levels were exceeded within any given three-year period.
[395] Opposition and efforts to repeal the legislation have drawn support from sources that include labor unions,[334][396] conservative advocacy groups,[397][398] Republicans, small business organizations and the Tea Party movement.
In Little Sisters of the Poor Saints Peter and Paul Home v. Pennsylvania, the Supreme Court ruled 7–2 on July 8, 2020, that employers with religious or moral objections to contraceptives can exclude such coverage from an employee's insurance plan.
[431] Democrats pointed out that the effect of invalidating the entire law would be to remove popular provisions such as the protection for preexisting conditions, and that the Republicans had still not offered any replacement plan—important issues in the 2020 elections.
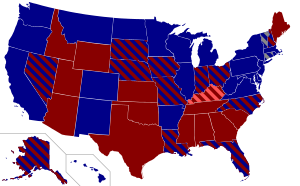
[435][436] For example, Missouri declined to expand Medicaid or establish a health insurance marketplace engaging in active non-cooperation, enacting a statute forbidding any state or local official to render any aid not specifically required by federal law.
[450][451][452] During a midnight congressional session starting January 11, the Senate of the 115th Congress of the United States voted to approve a "budget blueprint" that would allow Republicans to repeal parts of the law "without threat of a Democratic filibuster".
Finally, the "Health Care Freedom Act", nicknamed "skinny repeal" because it would have made the least change to ACA, failed by 49–51, with Collins, Murkowski, and McCain joining all Democrats and independents in voting against it.
[525] The show aired another sketch in September 2013 with Jay Pharoah as President Obama rolling out the plan to the public, and Aaron Paul and other cast members playing ordinary Americans helping him in advocating for the legislation.