Oncovirus
Other viruses are only carcinogenic when they integrate into the host cell genome as part of a biological accident, such as polyomaviruses and papillomaviruses.
For example, it has been shown that vFLIP and vCyclin interfere with the TGF-β signaling pathway indirectly by inducing oncogenic host mir17-92 cluster.
[12] Indirect viral oncogenicity involves chronic nonspecific inflammation occurring over decades of infection, as is the case for HCV-induced liver cancer.
Because foreign virus antigens are expressed in these tumors, persons who are immunosuppressed such as AIDS or transplant patients are at higher risk for these types of cancers.
[16] This phenomenon has been one of the major controversies of oncogenesis in the 20th century because an estimated 100 million people were inadvertently exposed to SV40 through polio vaccines.
[20] To drive the cell into S phase prematurely, the viruses must inactivate p53, which plays a central role in the G1/S checkpoint, as well as Rb, which, though downstream of it, is typically kept active by a positive feedback loop.
[22] DNA oncoviruses typically cause cancer by inactivating p53 and Rb, thereby allowing unregulated cell division and creating tumors.
In 1964, Howard Temin proposed a provirus hypothesis, but shortly after reverse transcription in the retrovirus genome was discovered.
Once inside the cell, the retrovirus goes through reverse transcription in the cytoplasm and generates a double-stranded DNA copy of the RNA genome.
Experimental and epidemiological data imply a causative role for viruses and they appear to be the second most important risk factor for cancer development in humans, exceeded only by tobacco usage.
19th century microbiology accumulated evidence that implicated bacteria, yeasts, fungi, and protozoa in the development of cancer.
But it was not recognized that cancer could have infectious origins until much later as virus had first been discovered by Dmitri Ivanovsky and Martinus Beijerinck at the close of the 19th century.
[43] The theory that cancer could be caused by a virus began with the experiments of Oluf Bang and Vilhelm Ellerman in 1908 at the University of Copenhagen.
Bang and Ellerman demonstrated that avian sarcoma leukosis virus could be transmitted between chickens after cell-free filtration and subsequently cause leukemia.
The reasons why chickens are so receptive to such transmission may involve unusual characteristics of stability or instability as they relate to endogenous retroviruses.
Genetic analysis of mice infected with Friend virus confirmed that retroviral integration could disrupt tumor suppressor genes, causing cancer.
[52] This compound was subsequently identified as a virus by Sarah Stewart and Bernice Eddy at the National Cancer Institute, after whom it was once called "SE polyoma".
[49] Though her findings received significant backlash, they were eventually accepted by the field and cemented the validity of viral oncogenesis.
Merck Laboratory also confirmed the existence of a rhesus macaque virus contaminating cells used to make Salk and Sabin polio vaccines.
Several years later, it was shown to cause cancer in Syrian hamsters, raising concern about possible human health implications.
[57][58] In 1964 Anthony Epstein, Bert Achong and Yvonne Barr identified the first human oncovirus from Burkitt's lymphoma cells.
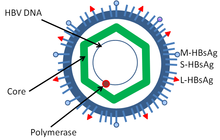
[59] In the mid-1960s Baruch Blumberg first physically isolated and characterized Hepatitis B while working at the National Institute of Health (NIH) and later the Fox Chase Cancer Center.
[60] Although this agent was the clear cause of hepatitis and might contribute to liver cancer hepatocellular carcinoma, this link was not firmly established until epidemiologic studies were performed in the 1980s by R. Palmer Beasley and others.
In 1981 Yorio Hinuma and his colleagues at Kyoto University reported visualization of retroviral particles produced by a leukemia cell line derived from patients with Adult T-cell leukemia/lymphoma.
[43] Between 1984 and 1986 Harald zur Hausen and Lutz Gissmann discovered HPV16 and HPV18, together these Papillomaviridae viruses (HPV) are responsible for approximately 70% of human papillomavirus infections that cause cervical cancers.
[65] In 1987 the Hepatitis C virus (HCV) was discovered by panning a cDNA library made from diseased tissues for foreign antigens recognized by patient sera.
This work was performed by Michael Houghton at Chiron, a biotechnology company, and Daniel W. Bradley at the Centers for Disease Control and Prevention (CDC).
[43] In 1994 Patrick S. Moore and Yuan Chang at Columbia University), working together with Ethel Cesarman,[67][68] isolated Kaposi's sarcoma-associated herpesvirus (KSHV or HHV8) using representational difference analysis.
This search was prompted by work from Valerie Beral and colleagues who inferred from the epidemic of Kaposi's sarcoma among patients with AIDS that this cancer must be caused by another infectious agent besides HIV, and that this was likely to be a second virus.