Pericoronitis
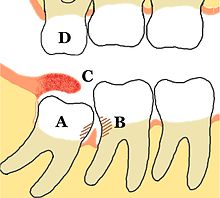
Pericoronitis is inflammation of the soft tissues surrounding the crown of a partially erupted tooth,[1] including the gingiva (gums) and the dental follicle.
[2] The soft tissue covering a partially erupted tooth is known as an operculum, an area which can be difficult to access with normal oral hygiene methods.
This infection can spread to the cheeks, orbits/periorbits, and other parts of the face or neck, and occasionally can lead to airway compromise (e.g. Ludwig's angina) requiring emergency hospital treatment.
The inflammation can be resolved by flushing the debris or infection from the pericoronal tissues or by removing the associated tooth or operculum.
Retaining the tooth requires improved oral hygiene in the area to prevent further acute pericoronitis episodes.
"[4] Systemic complications refers to signs and symptoms occurring outside of the mouth, such as fever, malaise or swollen lymph nodes in the neck.
In this scenario, pus may spontaneously discharge via an intra-oral sinus located over the mandibular second or first molar, or even the second premolar.
[13] A treatment controversy exists about the necessity and timing of the removal of asymptomatic, disease-free impacted wisdom teeth which prevents pericoronitis.
[14] Advocates for retaining wisdom teeth cite the risk and costs of unnecessary operations and the ability to monitor the disease through clinical exam and radiographs.
This is either through improved oral hygiene or by removal of the plaque stagnation areas through tooth extraction or gingival resection, which can be done with diode lasers atraumatically.
Irrigation may be assisted in conjunction with Debridement (removal of plaque, calculus and food debris) with periodontal instruments.
[4] A randomized clinical trial found green tea mouth rinse effective in controlling pain and trismus in acute cases of pericoronitis.
[18] Following treatment, if there are systemic signs and symptoms, such as facial or neck swelling, cervical lymphadenitis, fever or malaise, a course of oral antibiotics is often prescribed,.
[11] If there is dysphagia or dyspnoea (difficulty swallowing or breathing), then this usually means there is a severe infection and an emergency admission to hospital is appropriate so that intravenous medications and fluids can be administered and the threat to the airway monitored.
Removal is indicated when the involved tooth will not erupt any further due to impaction or ankylosis; if extensive work would be required to restore structural damage; or to allow improved oral hygiene.
[11] Extraction of teeth which are involved in pericoronitis carries a higher risk of dry socket, a painful complication which results in delayed healing.
However, when relying on just oral hygiene for impacted and partially erupted teeth, chronic pericoronitis with occasional acute exacerbation can be expected.
Even in people with normal immune function, pericoronitis may cause a spreading infection into the potential spaces of the head and neck.