Orthognathic surgery
Originally coined by Harold Hargis, it was more widely popularised first in Germany and then most famously by Hugo Obwegeser who developed the bilateral sagittal split osteotomy (BSSO).
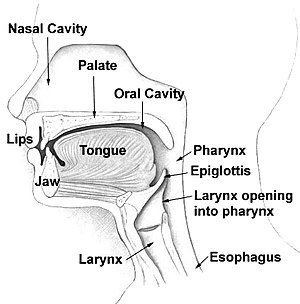
[2] Typically surgery is performed via the mouth, where jaw bone is cut, moved, modified, and realigned to correct malocclusion or dentofacial deformity.
A small number of mostly heavily socialist funded countries report that jaw correction procedures occur in some form or other in about 5% of a general population, but this figure would be at the extreme end of service [3][4][5] presenting with dentofacial deformities like maxillary prognathisms, mandibular prognathisms, open bites, difficulty chewing, difficulty swallowing, temporomandibular joint dysfunction pains, excessive wear of the teeth, and receding chins.
Increasingly, as people are more able to self-fund surgery, 3D facial diagnostic and design systems have emerged, as well as new operations that enable for a broad range of jaw correction procedures that have become readily accessible; in particularly in private maxillofacial surgical practice.
These procedures are replacing the traditional role of certain orthognathic surgery operations that have for decades served wholly and primarily orthodontic or dental purposes.
Prior to surgery, surgeons should take x-rays of the patient's jaw to determine the deformity, and to make a plan of procedures.
[11] Mandible osteotomies, or corrective jaw surgeries, benefit individuals who have difficulty chewing, swallowing, TMJ pains, excessive wear of the teeth, open bites, overbites, underbites, or a receding chin.
[13] Orthognathic surgery is a well established and widely used treatment option for insufficient growth of the maxilla in patients with an orofacial cleft.
[15] Patient reported aesthetic outcomes of orthognathic surgery for cleft lip and palate appear to be of overall satisfaction,[16][17] despite complications that may arise.
A potentially significant long-term outcome of orthognathic surgery is impaired maxillary growth, due to scar tissue formation.
Planning for the surgery usually involves input from a multidisciplinary team, including oral and maxillofacial surgeons, orthodontists, and occasionally a speech and language therapist.
Traditionally the presurgical orthodontic phase can take as long as one year and undertaken with conventional metal braces.
[33] However, these days new approaches and paradigms exist including surgery-first [34] And using clear aligner orthodontia (like Invisalign)[35][36] This procedure is used to correct mandible retrusion and mandibular prognathism (over and under bite).
Then, a chisel is inserted into the pre existing cuts and tapped gently in all areas to split the mandible of the left and right side.
If advancement is indicated for the chin, there are inert products available to implant onto the mandible, utilizing titanium screws, bypassing bone cuts.
[38][39] When a patient has a constricted (oval shape) maxilla, but normal mandible, many orthodontists request a rapid palatal expansion.
This consists of the surgeon making horizontal cuts on the lateral board of the maxilla, extending anterally to the inferior border of the nasal cavity.
Patients also may not drive or operate vehicles or large machinery during the consumption of painkillers, which are typically taken for six to eight days after the surgery, depending on the pain experienced.
In 1985, mandible and maxilla osteotomies were effectively used to correct more extreme deformities like receding chins, and to relieve pain from temporomandibular joint disorder (TMJ).
The study showed that 73% of patients developed an infection of the hardware inserted into the jaw when having their third molars removed during an osteotomy.
Prior to this, surgeons would fully sedate patients, hospitalizing them shortly after the surgery for a 2–3 day recovery, specifically from the anesthesia.
The original mandible and maxilla osteotomy procedure still remains almost unchanged, as it is the simplest and still the most effective for dentofacial deformity correction.