Partial androgen insensitivity syndrome
Treatment may include irreversible and far reaching surgical operations such as gonadectomy, as well as hormone replacement therapy, or vaginoplasty if the patient has desire to engage in penetrative sex.
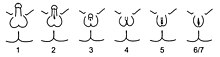
[3] The Quigley scale can be used in conjunction with the traditional three classes of AIS to provide additional information regarding the degree of genital masculinization, and is particularly useful when the diagnosis is PAIS.
Genital ambiguities are frequently detected during clinical examination at birth, and consequently, a PAIS diagnosis can be made during infancy as part of a differential diagnostic workup.
[20][21] Pubertal undervirilization is common, including gynecomastia, decreased secondary terminal hair, and/or a high pitched voice.
[29] Predominantly male phenotypes vary in the degree of genital undermasculinization to include micropenis, chordee, bifid scrotum, and/or pseudovaginal perineoscrotal hypospadias.
[3] Ambiguous phenotypic states include a phallic structure that is intermediate between a clitoris and a penis, and a single perineal orifice that connects to both the urethra and the vagina (i.e. urogenital sinus).
[53] Evidence of abnormal androgen binding in a genital skin fibroblast study has long been the gold standard for the diagnosis of PAIS,[3][54] even when an AR mutation is not present.
[1] The magnitude of the testosterone increase can help differentiate between androgen resistance and gonadal dysgenesis, as does evidence of a uterus on ultrasound examination.
[1] Testicular function can also be assessed by measuring serum anti-Müllerian hormone levels, which in turn can further differentiate PAIS from gonadal dysgenesis and bilateral anorchia.
Areas of management include sex assignment, genitoplasty, gonadectomy in relation to tumor risk, hormone replacement therapy, and genetic and psychological counseling.
[50] The decision of whether to raise an individual with PAIS as a boy or a girl may not be obvious; grades 3 and 4 in particular present with a phenotype that may be difficult to classify as primarily male or female, and some will be incapable of virilization at puberty.
[1][31][35] Parents of an affected newborn should seek immediate help at a center with an experienced multidisciplinary team, and should avoid gender assignment beforehand.
Some parents have pushed their children with intersex variations to display gender normative roles and behaviours, or to engage in hormonal and surgical interventions to make their bodies appear more aesthetically 'normative'.
[35] A genital skin fibroblast study [3][54] and a human chorionic gonadotropin (hCG) stimulation test [12] may also provide information helpful in the assessment of virilization capacity.
Psychosexual development is influenced by many factors, including the timing, amount, and type of androgen exposure, receptor functionality, and environment, and is thus difficult to predict.
[24][29][57][58][72] Gender assignment itself does not predicate the need for immediate genitoplasty; in some cases, surgical intervention can be delayed to allow the affected child to reach an age and maturity sufficient to have a role in such decisions.
[72] Scarring and tissue loss that result from repeated surgical procedures are of particular concern, due to the presumed negative impact on sexual function.
Both male and female participants cited the appearance of their genitalia as being the greatest contributing factor to their dissatisfaction with their body image.
[29] Additional surgeries may be required to correct postsurgical complications such as stenosis of the anastomosis between the native urethra and the graft, urethral fistulas, and posterior displacement of the balanic meatus.
[78] Procedures include clitoral reduction / recession, labiaplasty, repair of the common urogenital sinus, vaginoplasty, and vaginal dilation through non-surgical pressure methods.
[29] If PAIS presents with a common urogenital sinus, the American Academy of Pediatrics currently recommends that surgery to separate the urethra from the vagina be performed at an early age.
[47] Neovaginoplasty can be performed using skin grafts, a segment of bowel, ileum, peritoneum, Interceed,[80][81] buccal mucosa, amnion, or dura mater.
[29] Artificially induced puberty results in the same, normal development of secondary sexual characteristics, growth spurt, and bone mineral accumulation.
[17][84][85] Those undergoing high dose androgen therapy should be monitored for safety and efficacy of treatment, possibly including regular breast[17] and prostate[88] examinations.
[29] Adults with partial androgen insensitivity syndrome include Australian-Maltese advocate Tony Briffa, considered to be the world's first openly intersex mayor and public office-bearer.
[92][91][93][94][95][96][excessive citations] In history, the Roman sophist and philosopher Favorinus of Arelate has been described as having partial androgen insensitivity syndrome.
[97][98] In Sentencia SU-337/99, of May 12, 1999, the Constitutional Court of Colombia determined that "qualified and persistent" informed consent is required for genital surgeries in children.
The Court ruled in the case of XX, an 8-year old with ambiguous genitalia, androgen insensitivity and XY chromosomes, raised as a girl.
Doctors recommended feminizing surgeries, including a gonadectomy, vaginoplasty and clitoroplasty before puberty, but the hospital would not proceed without the consent of the Colombian Institute of Family Welfare and the Office of the Public Advocate.
Civil rights advocates and a minority of doctors favored deferring treatment due to lack of evidence and the irreversible nature of the proposed interventions.