Childhood acquired brain injury
Pediatric acquired brain injury (PABI) is the number one cause of death and disability for children and young adults in the United States.
They could also be caused by infections such as septicaemia; events such as anoxia and hypoxia occasioned by strangulation or near drowning, lead toxicity, and substance misuse.
It's very essential for a child to be able to enjoy fun childhood activities because it can help them build a social life, and easily interact with others.
[4] However, it is frequently the case that the functions associated with the damaged areas never fully develop and these deficits can present as significant disabilities or difficulties in later life.
[5] A significant proportion of the prior learning and the development of skills which has already taken place within an adult's brain can often be retained post injury.
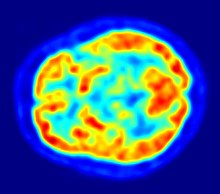
[1] Delayed physiological responses post-TBI can lead to neurodegeneration in various parts of the brain in both chronic and severe cases in children.
The parts of the brain that have been proven to be affected include: the hippocampus, amygdala, globus pallidus, thalamus, periventricular white matter, cerebellum, and brainstem.
[11] Children with moderate TBI only show some decline in attention and problem solving, but larger effects in visual immediate memory.
[10] Children with severe TBI are at higher risk for not achieving developmentally appropriate gains and not catching up with peers at school due to the crucial stage of learning at which their neural networks are disrupted by the injury.
Involvement in social situations is important for the normal development of children as a means of gaining an understanding of how to effectively work together with others.
Educational attainment and quality of life indicators for young adult survivors of childhood acquired brain injury are significantly lower than those of an uninjured peer group.
However caring and well meaning, the friends can also find it difficult to accommodate this new slowness into their usual give and take, resulting in the affected child being alienated and left out.
Another effect often seen as a result of damage to the vulnerable frontal lobes of a child's brain is 'disinhibition'[15] or a reduced ability to inhibit an impulse to say or do something long enough to calculate whether it's the correct or appropriate thing to say or do.
Disinhibition can also lead to sexually harmful behaviour, particularly when coupled with a lowered sense of risk and danger and a child with a brain injury can often become vulnerable to exploitation by peers or by strangers.
The loss of academic or sporting status, the indifference or antagonism of their peer group, the curtailing of their developing independence because of understandable parental worry, could all be experienced by a brain injured child or adolescent as almost a bereavement.
Siblings also could find it hard to come to terms with the loss of the brother or sister they knew and loved and with the amount of time, attention and emotional energy their parents have expended on the injured child.
Depending on how well informed another person is about the injury and about the nature of brain development, it can often be easy to ascribe aspects of a child's behaviour (or 'presentation') to the wrong underlying reason.
When the child fails to respond to what appears to be a straightforward instruction, for example 'put away your art work then go over there and get changed for PE', and is found still to be sitting at his desk five minutes later, the teacher might reach the conclusion that he is lazy or defiant.
Similarly, a child who has a visual impairment as a result of her injury could be mistaken for being clumsy and uncoordinated or just thoughtless, when she knocks over the milk jug or for being scatterbrained and inattentive when she neglects to complete the math problems written on the right hand side of the board.
"AIM is a 10-week, computerized treatment program that incorporates goal setting, the use of metacognitive strategies, and computer-based exercises designed to improve various aspects of attention.
The clinician's role is to select the specific, presenting mental areas that are impaired, as well as to modify the tasks and strategies in response to improvements of the patients' overtime.