Plasmodium falciparum
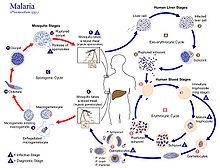
[2] The parasite is transmitted through the bite of a female Anopheles mosquito and causes the disease's most dangerous form, falciparum malaria.
These merozoites invade the erythrocytes (red blood cells) to form trophozoites, schizonts and gametocytes, during which the symptoms of malaria are produced.
The French Army physician Charles Louis Alphonse Laveran, while working at Bône Hospital (now Annaba in Algeria), correctly identified the parasite as a causative pathogen of malaria in 1880.
[11] The British physician Patrick Manson formulated the mosquito-malaria theory in 1894; until that time, malarial parasites were believed to be spread in air as miasma, a Greek word for pollution.
[14] P. falciparum is now generally accepted to have evolved from Laverania (a subgenus of Plasmodium found in apes) species present in gorillas in Western Africa.
[3][4] The closest relative of P. falciparum is P. praefalciparum, a parasite of gorillas, as supported by mitochondrial, apicoplastic and nuclear DNA sequences.
[21] Levels of genetic polymorphism are extremely low within the P. falciparum genome compared to that of closely related, ape infecting species of Plasmodium (including P.
The development of extensive agriculture likely increased mosquito population densities by giving rise to more breeding sites, which may have triggered the evolution and expansion of P.
These dots are Maurer's cleft and are secretory organelles that produce proteins and enzymes essential for nutrient uptake and immune evasion processes.
It contains secretory organelles called rhoptries and micronemes, which are vital for mobility, adhesion, host cell invasion, and parasitophorous vacuole formation.
[34] The sporozoites move in the bloodstream by gliding, which is driven by a motor made up of the proteins actin and myosin beneath their plasma membrane.
[37] Merozoites use the apicomplexan invasion organelles (apical complex, pellicle, and surface coat) to recognize and enter the host erythrocyte (red blood cell).
[40] After invading the erythrocyte, the parasite loses its specific invasion organelles (apical complex and surface coat) and de-differentiates into a round trophozoite located within a parasitophorous vacuole.
The trophozoite feeds on the haemoglobin of the erythrocyte, digesting its proteins and converting (by biocrystallization) the remaining heme into insoluble and chemically inert β-hematin crystals called haemozoin.
This gives rise to the characteristic clinical manifestations of falciparum malaria, such as fever and chills, corresponding to the synchronous rupture of the infected erythrocytes.
The male gametocyte undergoes a rapid nuclear division within 15 minutes, producing eight flagellated microgametes by a process called exflagellation.
[54] This discovery offers an opportunity to look into what could be playing a role in these behavior changes in mosquitoes and also find out what they ingest when they foraged on the selected plants.
In other studies, it has been shown that sources of sugars and some secondary metabolites e.g. ricinine, have contrasting effects on mosquito capacity to transmit the parasites malaria.
[46] The insoluble β-hematin crystal, haemozoin, produced from the digestion of haemoglobin of the RBCs is the main agent that affects body organs.
[71] The phagocytes can ingest free haemozoins liberated after the rupture of RBCs by which they are induced to initiate chains of inflammatory reaction that results in increased fever.
This difference is due to the ability of P. falciparum merozoites to invade a large number of RBCs sequentially without coordinated intervals, which is not seen in other malarial parasites.
Susceptibility to severe malaria is reduced in subsequent pregnancies due to increased antibody levels against variant surface antigens that appear on infected erythrocytes.
[78] P. falciparum works via sequestration, a process by which group of infected RBCs are clustered, which is not exhibited by any other species of malarial parasites.
[80] The mature schizonts change the surface properties of infected erythrocytes, causing them to stick to blood vessel walls (cytoadherence).
Death is caused by oxygen deprivation (hypoxia) due to inflammatory cytokine production and vascular leakage induced by the merozoites.
But medical programmes since the early 20th century, such as insecticide spraying, drug therapy, and environmental engineering, resulted in complete eradication in the 1970s.
[107] According to WHO guidelines 2010,[108] artemisinin-based combination therapies (ACTs) are the recommended first-line antimalarial treatments for uncomplicated malaria caused by P. falciparum.
[111] The International Agency for Research on Cancer (IARC) has classified malaria due to P. falciparum as a Group 2A carcinogen, meaning that the parasite is probably a cancer-causing agent in humans.
[117] This, in turn, activates an enzyme called activation-induced cytidine deaminase (AID), which tends to cause mutation in the DNA (by double-strand break) of EBV-infected lymphocytes.
[119][120] E. A. Beet, a doctor working in Southern Rhodesia (now Zimbabwe) had observed in 1948 that sickle-cell disease was related to a lower rate of malaria infections.