Plasmodium knowlesi
P. knowlesi malaria is an emerging disease previously thought to be rare in humans, but increasingly recognized as a major health burden in Southeast Asia.
These include the large bulbous rhoptries, smaller micronemes, and dispersed dense granules, each of which secretes effectors to enter and modify the host cell.
[6][7] Like other apicomplexans, P. knowlesi also has two organelles of endosymbiotic origin: a single large mitochondrion and the apicoplast, both of which are involved in the parasite's metabolism.
[8] Despite its morphological similarity to P. malariae, P. knowlesi is most closely related to P. vivax as well as other Plasmodium species that infect non-human primates.
[14] Laboratory tests of infected people nearly always show a low platelet count, although this rarely leads to bleeding problems.
[14] As disease progresses, parasites replicate to very high levels in the blood likely causing acute kidney injury, jaundice, shock, and respiratory distress.
[11] Malaria is traditionally diagnosed by examining Giemsa-stained blood films under a microscope; however, differentiating P. knowlesi from other Plasmodium species in this way is challenging due to their similar appearance.
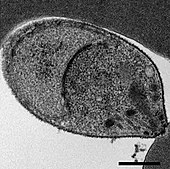
[11] P. knowlesi ring-stage parasites stained with Giemsa resemble P. falciparum ring stages, appearing as a circle with one or two dark dots of chromatin.
[18] Older trophozoites appear more dispersed, forming a rectangular-shape spread across the host cell called a "band-form" that resembles the similar stage in P.
[18] Schizonts appear, similarly to other Plasmodium species, as clusters of purple merozoites surrounding a central dark-colored pigment.
[18] Due to the morphological similarity among Plasmodium species, misdiagnosis of P. knowlesi infection as P. falciparum, P. malariae, or P. vivax is common.
[11] Because P. knowlesi takes only 24 hours to complete its erythrocytic cycle, it can rapidly result in very high levels of parasitemia with fatal consequences.
[17] For those with uncomplicated malaria, the World Health Organization recommends treatment with artemisinin-based combination therapy (ACT) or chloroquine.
[20] For those with severe malaria, the World Health Organization recommends administration of intravenous artesunate for at least 24 hours, followed by ACT treatment.
[11] Infection with P. knowlesi is associated with socioeconomic and lifestyle factors that bring people into the dense forests where the mosquito hosts are commonly found.
[14] P. knowlesi has long been used as a research model for studying the interaction between parasite and host, and developing antimalarial vaccines and drugs.
Isolated sporozoites can infect primary rhesus hepatocytes, allowing the in vitro study of the parasite liver stage.
[10] Additionally, P. knowlesi and P. falciparum are the only Plasmodium species that can be maintained continuously in cultured red blood cells, both rhesus and human.
[10] P. knowlesi can be genetically modified in the lab by transfection either in the rhesus macaque model system, or in blood cell culture.
[1] The Italian physician Giuseppe Franchini first described what may have been P. knowlesi in 1927 when he noted a parasite distinct from P. cynomolgi and P. inui in the blood of a long-tailed macaque.
[3][26] Also in 1932, John Sinton and H. W. Mulligan further described the morphology of the parasite in blood cells, determined it to be a distinct species from others described, and named it Plasmodium knowlesi in honor of Robert Knowles.
[3] Soon thereafter, in 1935 C. E. Van Rooyen and George R. Pile reported using P. knowlesi infection to treat general paralysis in psychiatric patients.