Polio eradication
[1] These organizations, along with the U.S. Centers for Disease Control and Prevention (CDC) and The Gates Foundation, have spearheaded the campaign through the Global Polio Eradication Initiative (GPEI).
[16] Attenuated poliovirus derived from the oral polio vaccine is excreted, infecting and indirectly inducing immunity in unvaccinated individuals, and thus amplifying the effects of the doses delivered.
As a result of such circulating vaccine-derived poliovirus (cVDPV) strains, polio outbreaks have periodically recurred in regions that have long been free of the wild virus, but where vaccination rates have fallen.
Oral vaccines can also give rise to persistent infection in immunodeficient individuals, with the virus eventually mutating into a more virulent immunodeficiency-associated vaccine-derived poliovirus (iVDPV).
These vaccines are more expensive and more difficult to deliver, and they lack the ability to induce contact immunity because they contain only killed virus, but they likewise are incapable of giving rise to vaccine-derived viral strains.
[34] Among the greatest obstacles to global polio eradication are the lack of basic health infrastructure, which limits vaccine distribution and delivery, the crippling effects of civil war and internal strife, and the sometimes oppositional stance that marginalized communities take against what is perceived as a potentially hostile intervention by outsiders.
In India, the major challenge appeared to be the high efficiency of transmission within the populations of Bihar and Uttar Pradesh states, set against the low (~80% after three doses against type 1) seroconversion response seen from the vaccine.
In those countries where international spread from endemic countries had resulted in the reestablishment of transmission, namely Angola, Chad, and South Sudan, the key issues identified were underdeveloped health systems and low routine vaccine coverage, although the low level of resources committed to Angola and South Sudan for the purpose of curtailing the spread of polio and climatic factors was also identified as playing a role.
[46][47] Concerns were addressed through extensive outreach, directed both toward the communities involved and respected clerical bodies, as well as promoting local ownership of the eradication campaign in each region.
[43] Skepticism in the Muslim world was exacerbated when it was learned that in 2011 the Central Intelligence Agency (CIA) had conducted a fake hepatitis B immunization campaign, hoping to collect blood samples from Osama bin Laden's compound in Abbottabad in order to confirm the genetic identity of the children living there, and by implication his own presence, leading directly to his killing.
In Nigeria this has taken the form of 'block rejection' of vaccination that is only resolved when state officials agree to repair or improve schools and health-care facilities, pave roads or install electricity.
The number of planned polio vaccination campaigns had recently been reduced, and populations in northern India, particularly from the Islamic background, engaged in mass resistance to immunization.
However, by 2004, India had adopted strategies to increase ownership of polio vaccinations in marginalized populations, and the immunity gap in vulnerable groups rapidly closed.
In addition to the rumors of sterility and the ban by Nigeria's Kano state, civil war and internal strife in Sudan and Côte d'Ivoire have complicated WHO's polio eradication goal.
In summer 2005, the WHO, UNICEF and the Indonesian government made new efforts to lay the fears to rest, recruiting celebrities and religious leaders in a publicity campaign to promote vaccination.
The poliovirus type 1 infection occurred in an unvaccinated, immunocompromised infant girl aged seven months (the index patient) in an Amish community whose members predominantly were not vaccinated for polio.
Officials credit the drop in new infections to improved political control in the southern states and resumed immunisation in the north, where Muslim clerics led a boycott of vaccination in late 2003.
The plan called for mass immunization campaigns in the three remaining endemic countries, and also dictated a switch to inactivated virus injections, to avoid the risk of the vaccine-derived outbreaks that occasionally occur from use of the live-virus oral vaccine.
[121][122] On 27 March 2014, the WHO announced the eradication of poliomyelitis in the South-East Asia Region, in which the WHO includes eleven countries: Bangladesh, Bhutan, North Korea, India, Indonesia, Maldives, Myanmar, Nepal, Sri Lanka, Thailand, and Timor-Leste.
[131] A small number of additional cases in Nigeria, caused by WPV1, were viewed as a setback, the first being detected there in almost two years, yet the virus had been circulating undetected in regions inaccessible due to the activities of Boko Haram.
In spite of a significant drop in detected cases in Pakistan, there was an increase in the percentage of environmental samples that test positive for the polio virus, suggesting gaps in identification of infected individuals.
[140] Laos was declared free of cVDPV1 in March 2017,[61][141] but three distinct cVDPV2 outbreaks occurred in the Democratic Republic of the Congo, one of them of recent origin, the other two having circulated undetected for more than a year.
[142][143][144][145] In Syria, a large outbreak began at Mayadin, Deir ez-Zor Governorate, a center of fighting in the Syrian Civil War, and also spreading to neighboring districts saw 74 confirmed cases from a viral strain that had circulated undetected for about two years.
[151][171] In the third remaining country in which polio was classified as endemic, Nigeria, wild poliovirus has not been detected since October 2016, and levels of AFP surveillance are sufficient, even in security-compromised regions, to suggest transmission of WPV may have been interrupted.
[172] In addition to eighteen reported paralysis cases in Nigeria, the cVDPV2 outbreaks there spread to Benin, Burkina Faso, Chad, Ghana, Niger, and Togo, while the virus was also detected in environmental samples from Cameroon and Ivory Coast.
[179] Additional challenges were a conspiracy theory circulating on social media claiming that the polio vaccine contained coronavirus, and moves by President Donald Trump of the United States to cut funding for the World Health Organization.
[4] WHO Director-General Tedros Adhanom called it a "great day... but not the end of polio",[184] as there remain major continuing outbreaks of vaccine-derived poliovirus in West Africa and Ethiopia in addition to wild cases in Afghanistan and Pakistan.
[186] The Independent Monitoring Board of the GPEI in its September 2023 Report [211] mentioned a continued, geographically restricted, endemic transmission in the east of Afghanistan and in the southern districts of Pakistan's Khyber Pakhtunkhwa province.
In addition eighteen countries have had positive environmental samples of cVDPV2 but no confirmed cases: Algeria, Cote D'Ivoire, Djibouti, Egypt, Equatorial Guinea, Finland, Gambia, Germany, Ghana, Kenya, Mozambique, Poland, Senegal, Sierra Leone, Spain, Sudan, Uganda, United Kingdom and Zimbabwe.
[213][214] Beginning at certification of WPV eradication, the post-certification strategy will come into effect,[215]: 6 with program priorities shifting towards outbreak preparedness and containment of existing virus material rather than circulating disease.




|
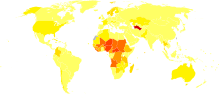
no data
<0.3
0.3–0.75
0.75–1.2
1.2–1.65
1.65–2.1
2.1–2.55
|
2.55–3
3–4
4–5
5–7.5
7.5–10
>10
|











