Post-traumatic epilepsy
[3] People with head trauma may remain at a higher risk for post-traumatic seizures than the general population even decades after the injury.
[9] Modern surgical techniques for PTE have their roots in the 19th century, but trepanation (cutting the skull to make a hole) may have been used for the condition in ancient cultures.
A provoked seizure is one that results from an exceptional, nonrecurring cause such as the immediate effects of trauma rather than a defect in the brain; it is not an indication of epilepsy.
[7] The haptoglobin Hp2-2 allele may be another genetic risk factor, possibly because it binds hemoglobin poorly and thus allows more iron to escape and damage tissues.
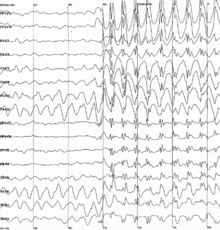
[19] Evidence suggests that mild head injuries do not confer an increased risk of developing PTE, while more severe types do.
[21] One study found that the 30-year risk of developing PTE was 2.1% for mild TBI, 4.2% for moderate, and 16.7% for severe injuries, as shown in the chart at right.
[27] The iron from blood also reduces the activity of an enzyme called nitric oxide synthase, another factor thought to contribute to PTE.
[8] TBI may lead to the excessive release of glutamate and other excitatory neurotransmitters (those that stimulate brain cells and increase the likelihood that they will fire).
This excessive glutamate release can lead to excitotoxicity, damage to brain cells through overactivation of the biochemical receptors that bind and respond to excitatory neurotransmitters.
[4] Neurons that are in a hyperexcitable state due to trauma may create an epileptic focus in the brain that leads to seizures.
[2][3][7][33] Why antiepileptic drugs in clinical trials have failed to stop PTE from developing is not clear, but several explanations have been offered.
[7] Animal studies have similarly failed to show much protective effect of the most commonly used seizure medications in PTE trials, such as phenytoin and carbamazepine.
[19] However, it has been proposed that a narrow window of about one hour after TBI may exist during which administration of antiepileptics could prevent epileptogenesis (the development of epilepsy).
[34] The antiepileptics carbamazepine and valproate are the most common drugs used to treat PTE; phenytoin may also be used but may increase risk of cognitive side effects such as impaired thinking.
[12] Among antiepileptic drugs tested for seizure prevention after TBI (phenytoin, valproic acid, carbamazepine, phenobarbital), no evidence from randomized controlled trials has shown superiority of one over another.
[8] People whose PTE does not respond to medication may undergo surgery to remove the epileptogenic focus, the part of the brain that is causing the seizures.
[8] It can be particularly difficult in PTE to localize the epileptic focus, in part because TBI may affect diffuse areas of the brain.
[4] When there are multiple epileptic foci or the focus cannot be localized, and drug therapy is not effective, vagus nerve stimulation is another option for treating PTE.
[31] People with PTE have follow-up visits, in which health care providers monitor neurological and neuropsychological function and assess the efficacy and side effects of medications.
[8] As with other types of epilepsy, individuals with PTE are advised to exercise caution when performing activities for which seizures could be particularly risky, such as rock climbing.
[12] PTE has also been found to be associated with worse social and functional outcomes but not to worsen patients' rehabilitation or ability to return to work.
[8] However, people with PTE may have trouble finding employment if they admit to having seizures, especially if their work involves operating heavy machinery.
[10] The French-educated American surgeon Benjamin Winslow Dudley (1785–1870) performed six trepanations for PTE between the years of 1819 and 1832 in Kentucky and had good results despite the unavailability of antisepsis.
[40] The surgery involved opening the skull at the site of injury, debriding injured tissue, and sometimes draining blood or fluid from under the dura mater.
[40] Dudley's work was the largest series of its kind that had been done up to that point, and it encouraged other surgeons to use trepanation for post-traumatic seizures.
[40] His reports on the operations came before it was accepted that surgery to relieve excess pressure within the skull was effective in treating epilepsy, but it helped set the stage for trepanation for PTE to become common practice.
[10] Surgery was the standard treatment for PTE until the years following World War II, when the condition received more attention as soldiers who had survived head trauma developed it.
[12] How epilepsy develops after an injury to the brain is not fully understood, and gaining such understanding may help researchers find ways to prevent it, or make it less severe or easier to treat.
[22] Researchers hope to identify biomarkers, biological indications that epileptogenesis is occurring, as a means to find drugs that can target pathways by which epilepsy develops.
[31] An increase in understanding of age differences in epilepsy development after trauma may also help researchers find biomarkers of epileptogenesis.