Primary sclerosing cholangitis
Genetic susceptibility, immune system dysfunction, and abnormal composition of the gut flora may play a role.
[7] The disease was initially described in the mid-1800s, but was not fully characterized until the 1970s with the advent of improved medical-imaging techniques such as endoscopic retrograde cholangiopancreatography.
[11][12] Data have provided novel insights suggesting: In addition, longstanding, well-recognized associations are seen between PSC and human leukocyte antigen alleles (A1, B8, and DR3).
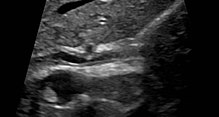
[citation needed] PSC is generally diagnosed on the basis of having at least two of three clinical criteria after secondary causes of sclerosing cholangitis have been ruled out:[citation needed] Historically, a cholangiogram would be obtained via endoscopic retrograde cholangiopancreatography (ERCP), which typically reveals "beading" (alternating strictures and dilation) of the bile ducts inside and/or outside the liver.
MRCP has unique strengths, including high spatial resolution, and can even be used to visualize the biliary tract of small animal models of PSC.
[24] Primary sclerosing cholangitis and primary biliary cholangitis are distinct entities and exhibit important differences, including the site of tissue damage within the liver, associations with IBD, which includes ulcerative colitis and Crohn's disease, response to treatment, and risks of disease progression.
[25] Primary sclerosing cholangitis is typically classified into three subgroups based on whether the small and/or large bile ducts are affected.
[30] ERCP and specialized techniques may also be needed to help distinguish between a benign PSC stricture and a bile-duct cancer (cholangiocarcinoma).
Indications for transplantation include recurrent bacterial ascending cholangitis, decompensated cirrhosis, hepatocellular carcinoma, hilar cholangiocarcinoma, and complications of portal hypertension.
[38][39] Association was demonstrated between anti-GP2 IgA and progressive liver fibrosis, cholangiocarcinoma development and shorter transplantation free survival in PSC patients.
[35] Other markers which may be measured and monitored are a complete blood count, serum liver enzymes, bilirubin levels (usually grossly elevated), kidney function, and electrolytes.
[citation needed] Similarly, a screening colonoscopy is recommended in people who receive a new diagnosis of primary sclerosing cholangitis since their risk of colorectal cancer is 10 times higher than that of the general population.
[1] PSC is strongly associated with IBD, in particular ulcerative colitis (UC) and to a lesser extent Crohn's disease.
[19] Of note, the presence of colitis appears to be associated with a greater risk of liver disease progression and bile duct cancer (cholangiocarcinoma) development, although this relationship remains poorly understood.
[19] PSC can affect men and women at any age, although it is commonly diagnosed in the fourth decade of life, most often in the presence of IBD.
[18] PSC progresses slowly and is often asymptomatic, so it can be present for years before it is diagnosed and before it causes clinically significant consequences.