Purple urine bag syndrome
[5] The purple discoloration is harmless and can be resolved with treatments targeted to specific bacteria or any underlying medical conditions.
[7] Treatment also consists of providing comfort to both patients and their family, administering antibiotics and performing regular catheter changes.
The prognosis is good, however, the morbidity and mortality rates associated with PUBS are elevated depending on patient's underlying health status.
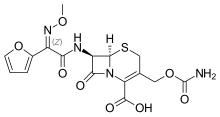
[10] Purple urine bag syndrome (PUBS) is thought to be caused by tryptophan from the diet being metabolized by bacteria in the gastrointestinal tract to produce indole.
In purple urine bag syndrome, bacterial enzymes that colonize the urinary catheter, specifically sulfatases and phosphotases, convert indoxyl sulfate to the colored compounds indirubin and indigo.
[12] The change in tryptophan metabolism is theorized to be due to diminished gut motility resulting in prolonged transit times.
A common side effect of overuse of laxatives is damage to the colorectal mucosal lining and changes to the normal intestinal microbiota.
The most common bacteria found to be responsible are Providencia stuartti and rettgeri, Proteus mirabilis, Pseudomonas auruginosa, Klebsiella pneumoniae, Escherichia coli, Morganella, and citrobacter species, Enterococci, and Group B Streptococci.
[14] Purple urine bag syndrome can be a side effect of having a urinary tract infection while using a catheter for a long period of time.
However, it is important that these facilities use clean tools that have been properly disinfected when handling and processing the meat to avoid any accidental transmission.
[17] P. aeruginosa is a bacteria that was first discovered due to its ability to cause the surgical dressings and bandages of patients to turn a blue/green color.
E. coli has the ability to cause a wide variety of illnesses in humans including diarrhea, sepsis, meningitis (inflammation of the membranes surrounding the brain and spinal cord), and urinary tract infections.
[24] Despite the seemingly harmless nature of PUBS, it is important to treat immediately in order to stop progression to more dangerous conditions.
In the case of an elderly woman with limited mobility due to a previous fracture, she was put on a catheter, a tube that provides hospital patients with fluids and nutrients as they recover.
[25] Another case focuses on the development of purple urine bag syndrome within a middle aged Pakistani woman who exhibited several risk factors such as enduring constipation (a long-lasting health issue indicating decreased excretion of fecal matter), use of a catheter for an extended period of time, as well as being female.
[2] She experienced symptoms of purple urine bag syndrome frequently, and each time she was given oral antibiotics to treat the potential underlying cause which was surmised to be a urinary tract infection.
[2] Once the woman came to a specific facility, she was started on the antibiotic cefixime by mouth and was prescribed lactulose to relieve constipation, a risk factor of purple urinary bag syndrome.
[2] Despite all of this, it is important to note that purple urine bag syndrome is generally harmless and does not require immediate treatment usually unless progressing to a serious state within the patient.
[7] Purple urine bag syndrome is associated with longer periods using a catheter as well as has greater prevalence among those who have trouble with making bowel movements or are dehydrated (lacking adequate fluid).
[27] In terms of bowel movements, it is encouraged to promote gut health, by doing certain activities like exercising and consuming lots of fluids and fiber.
Besides consuming large amounts of fluid and fiber, avoiding sugar, caffeine, and alcohol, taking cranberry pills, and exercising, it is recommended to frequently use the restroom to clear the bladder, urinate after sexual intercourse, and lastly wipe your underside thoroughly to prevent the spread of bacteria to your private parts; all of these tips will ultimately prevent the development of UTI's and furthermore decrease the likelihood of attaining purple urine bag syndrome.
[30] From October 1980 to August 2016, reported PUBS cases were analyzed in a systemic review to make comparisons between patient age, gender, co-morbidities, vital signs, laboratory test results, and mortality.
[30] In particular, the parameters that were evaluated were urine pH value, presence of fever, shock, WBC count, constipation, and co-morbidities like diabetes and uremia.
[32] From this case report, it was confirmed that the following are primary risk factors for PUBS: female gender, increased dietary tryptophan (ex.
bananas, meat), long-term immobilization and catheterization, severe constipation, high urinary bacterial load, and renal failure.
[25] The Foley catheter was replaced, the purple urine disappeared, and the urinalysis was sterile; as a result, the patient was discharged in stable conditions.