Radiology
Interventional radiology is the performance of usually minimally invasive medical procedures with the guidance of imaging technologies such as those mentioned above.
[3] The radiographer, also known as a "radiologic technologist" in some countries such as the United States and Canada, is a specially trained healthcare professional that uses sophisticated technology and positioning techniques to produce medical images for the radiologist to interpret.
Due to its availability, speed, and lower costs compared to other modalities, radiography is often the first-line test of choice in radiologic diagnosis.
[citation needed] Mammography and DXA are two applications of low energy projectional radiography, used for the evaluation for breast cancer and osteoporosis, respectively.
These radiocontrast agents strongly absorb or scatter X-rays, and in conjunction with the real-time imaging, allow demonstration of dynamic processes, such as peristalsis in the digestive tract or blood flow in arteries and veins.
[citation needed] Spiral multidetector CT uses 16, 64, 254 or more detectors during continuous motion of the patient through the radiation beam to obtain fine detail images in a short exam time.
[citation needed] The introduction of computed tomography in the early 1970s revolutionized diagnostic radiology by providing front-line clinicians with detailed images of anatomic structures in three dimensions.
[citation needed] Medical ultrasonography uses ultrasound (high-frequency sound waves) to visualize soft tissue structures in the body in real time.
No ionizing radiation is involved, but the quality of the images obtained using ultrasound is highly dependent on the skill of the person (ultrasonographer) performing the exam and the patient's body size.
Examinations of larger, overweight patients may have a decrease in image quality as their subcutaneous fat absorbs more of the sound waves.
The progression of pregnancies can be thoroughly evaluated with less concern about damage from the techniques employed, allowing early detection and diagnosis of many fetal anomalies.
A clot, embedded deep in one of the inner veins of the legs, can be found via ultrasound before it dislodges and travels to the lungs, resulting in a potentially fatal pulmonary embolism.
An advantage of MRI is its ability to produce images in axial, coronal, sagittal and multiple oblique planes with equal ease.
With advances in scanning speed and spatial resolution, and improvements in computer 3D algorithms and hardware, MRI has become an important tool in musculoskeletal radiology and neuroradiology.
[citation needed] One disadvantage is the patient has to hold still for long periods of time in a noisy, cramped space while the imaging is performed.
Nuclear medicine imaging involves the administration into the patient of radiopharmaceuticals consisting of substances with affinity for certain body tissues labeled with radioactive tracer.
The heart, lungs, thyroid, liver, brain, gallbladder, and bones are commonly evaluated for particular conditions using these techniques.
In the most modern devices, nuclear medicine images can be fused with a CT scan taken quasisimultaneously, so the physiological information can be overlaid or coregistered with the anatomical structures to improve diagnostic accuracy.
[citation needed] The fusion technology has gone further to combine PET and MRI similar to PET and CT. PET/MRI fusion, largely practiced in academic and research settings, could potentially play a crucial role in fine detail of brain imaging, breast cancer screening, and small joint imaging of the foot.
The technology recently blossomed after passing the technical hurdle of altered positron movement in strong magnetic field thus affecting the resolution of PET images and attenuation correction.
[citation needed] The basic concept behind interventional radiology is to diagnose or treat pathologies, with the most minimally invasive technique possible.
By minimizing the physical trauma to the patient, peripheral interventions can reduce infection rates and recovery times, as well as hospital stays.
To be a trained interventionalist in the United States, an individual completes a five-year residency in radiology and a one- or two-year fellowship in IR.
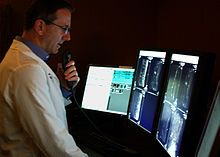
In these cases, the images can be sent across time zones (e.g. to Spain, Australia, India) with the receiving Clinician working his normal daylight hours.
In the U.S., many hospitals outsource their radiology departments to radiologists in India due to the lowered cost and availability of high speed internet access.
The major advantage of teleradiology is the ability to use different time zones to provide real-time emergency radiology services around-the-clock.
[17] Radiology is a field in medicine that has expanded rapidly after 2000 due to advances in computer technology, which is closely linked to modern imaging techniques.
Although previously taken in Chicago or Tucson, Arizona, beginning in February 2021, the computer test transitioned permanently to a remote format.
[citation needed] Veterinary radiologists are veterinarians who specialize in the use of X-rays, ultrasound, MRI and nuclear medicine for diagnostic imaging or treatment of disease in animals.
During the first year of training, radiology trainees are expected to pass the first part of the Fellowship of the Royal College of Radiologists (FRCR) exam.