Radiosurgery
Radiosurgery was originally defined by the Swedish neurosurgeon Lars Leksell as "a single high dose fraction of radiation, stereotactically directed to an intracranial region of interest".
[3] Stereotactic radiosurgery was first developed in 1949 by the Swedish neurosurgeon Lars Leksell to treat small targets in the brain that were not amenable to conventional surgery.
Ten years later significant progress had been made, due in considerable measure to the contribution of the physicists Kurt Liden and Börje Larsson.
This second Gamma Knife unit was designed to produce spherical lesions to treat brain tumors and intracranial arteriovenous malformations (AVMs).
In 1982, the Spanish neurosurgeon J. Barcia-Salorio began to evaluate the role of cobalt-generated and then Linac-based photon radiosurgery for the treatment of AVMs and epilepsy.
[14] Winston and Lutz further advanced Linac-based radiosurgical prototype technologies by incorporating an improved stereotactic positioning device and a method to measure the accuracy of various components.
[citation needed] Technological improvements in medical imaging and computing have led to increased clinical adoption of stereotactic radiosurgery and have broadened its scope in the 21st century.
In the 21st century the original concept of radiosurgery expanded to include treatments comprising up to five fractions, and stereotactic radiosurgery has been redefined as a distinct neurosurgical discipline that utilizes externally generated ionizing radiation to inactivate or eradicate defined targets, typically in the head or spine, without the need for a surgical incision.
Fractionated radiotherapy relies more heavily on the different radiosensitivity of the target and the surrounding normal tissue to the total accumulated radiation dose.
[20] Historically, the field of fractionated radiotherapy evolved from the original concept of stereotactic radiosurgery following discovery of the principles of radiobiology: repair, reassortment, repopulation, and reoxygenation.
Systems designed to complement conventional Linacs with beam-shaping technology, treatment planning, and image-guidance tools to provide.
Significant clinical judgment must be used with this technique and considerations must include lesion type, pathology if available, size, location and age and general health of the patient.
Since radiosurgery does not remove the tumor but inactivates it biologically, lack of growth of the lesion is normally considered to be treatment success.
[29] The selection of the proper kind of radiation and device depends on many factors including lesion type, size, and location in relation to critical structures.
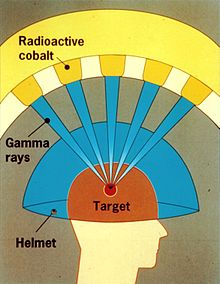
A Gamma Knife typically contains 201 cobalt-60 sources of approximately 30 curies each (1.1 TBq), placed in a hemispheric array in a heavily shielded assembly.
The patient wears a specialized helmet that is surgically fixed to the skull, so that the brain tumor remains stationary at the target point of the gamma rays.
Gamma Knife therapy, like all radiosurgery, uses doses of radiation to kill cancer cells and shrink tumors, delivered precisely to avoid damaging healthy brain tissue.
Each individual beam is of relatively low intensity, so the radiation has little effect on intervening brain tissue and is concentrated only at the tumor itself.
Long-term follow-up data has shown it to be as effective as radiofrequency ablation, but inferior to surgery in preventing the recurrence of pain.
[citation needed] As of 2013[update] there was no evidence that proton beam therapy is better than any other types of treatment in most cases, except for a "handful of rare pediatric cancers".
Critics, responding to the increasing number of very expensive PBT installations, spoke of a "medical arms race" and "crazy medicine and unsustainable public policy".