Radiation therapy
The precise treatment intent (curative, adjuvant, neoadjuvant therapeutic, or palliative) will depend on the tumor type, location, and stage, as well as the general health of the patient.
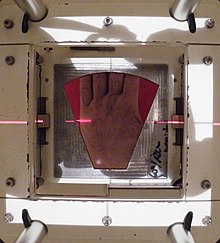
Brachytherapy, in which a radioactive source is placed inside or next to the area requiring treatment, is another form of radiation therapy that minimizes exposure to healthy tissue during procedures to treat cancers of the breast, prostate, and other organs.
[48] High doses of radiation during pregnancy induce anomalies, impaired growth and intellectual disability, and there may be an increased risk of childhood leukemia and other tumors in the offspring.
In 2010 the American Society for Radiation Oncology (ASTRO) launched a safety initiative called Target Safely that, among other things, aimed to record errors nationwide so that doctors can learn from each and every mistake and prevent them from recurring.
[55] Much research has been devoted to overcoming hypoxia including the use of high pressure oxygen tanks, hyperthermia therapy (heat therapy which dilates blood vessels to the tumor site), blood substitutes that carry increased oxygen, hypoxic cell radiosensitizer drugs such as misonidazole and metronidazole, and hypoxic cytotoxins (tissue poisons), such as tirapazamine.
Newer research approaches are currently being studied, including preclinical and clinical investigations into the use of an oxygen diffusion-enhancing compound such as trans sodium crocetinate as a radiosensitizer.
[56] Charged particles such as protons and boron, carbon, and neon ions can cause direct damage to cancer cell DNA through high-LET (linear energy transfer) and have an antitumor effect independent of tumor oxygen supply because these particles act mostly via direct energy transfer usually causing double-stranded DNA breaks.
[57] This difference is very important in cases where the close proximity of other organs makes any stray ionization very damaging (example: head and neck cancers).
This X-ray exposure is especially bad for children, due to their growing bodies, and while depending on a multitude of factors, they are around 10 times more sensitive to developing secondary malignancies after radiotherapy as compared to adults.
The rationale of hypofractionation is to reduce the probability of local recurrence by denying clonogenic cells the time they require to reproduce and also to exploit the radiosensitivity of some tumors.
[66] The content and variation of manganese (measurable by electron paramagnetic resonance) were found to be good predictors of radiosensitivity, and this finding extends also to human cells.
[67] An association was confirmed between total cellular manganese contents and their variation, and clinically inferred radioresponsiveness in different tumor cells, a finding that may be useful for more precise radiodosages and improved treatment of cancer patients.
The worry is that some high-dose treatments may be limited by the radiation toxicity capacity of healthy tissues which lie close to the target tumor volume.
An example of this problem is seen in radiation of the prostate gland, where the sensitivity of the adjacent rectum limited the dose which could be safely prescribed using 2DXRT planning to such an extent that tumor control may not be easily achievable.
Prior to the invention of the CT, physicians and physicists had limited knowledge about the true radiation dosage delivered to both cancerous and healthy tissue.
Brand names for these treatments include Axesse, Cyberknife, Gamma Knife, Novalis, Primatom, Synergy, X-Knife, TomoTherapy, Trilogy and Truebeam.
Proof of improved survival benefit from either of these two techniques over conventional radiation therapy (2DXRT) is growing for many tumor sites, but the ability to reduce toxicity is generally accepted.
This is particularly the case for head and neck cancers in a series of pivotal trials performed by Professor Christopher Nutting of the Royal Marsden Hospital.
[80] The implantable device can also be a small wireless transmitter sending out an RF signal which then will be received by a sensor array and used for localization and real-time tracking of the tumor position.
[83] While solutions to this issue have been developed, which either reduce the TG effect to negligible amounts or remove it completely, they depend upon the method of IMRT being used and some of them carry costs of their own.
[84] Volumetric modulated arc therapy (VMAT) is a radiation technique introduced in 2007[85] which can achieve highly conformal dose distributions on target volume coverage and sparing of normal tissues.
VMAT has an advantage in patient treatment, compared with conventional static field intensity modulated radiotherapy (IMRT), of reduced radiation delivery times.
The application of this technique, which has yet to be automated, has been described carefully to enhance the ability of departments to perform it, and in 2021 it was reported as feasible in a small clinical trial,[90] though its efficacy has yet to be formally studied.
Auger therapy (AT) makes use of a very high dose[97] of ionizing radiation in situ that provides molecular modifications at an atomic scale.
[111] As one example of the localized nature of breast brachytherapy, the SAVI device delivers the radiation dose through multiple catheters, each of which can be individually controlled.
This approach decreases the exposure of healthy tissue and resulting side effects, compared both to external beam radiation therapy and older methods of breast brachytherapy.
[118] Medicine has used radiation therapy as a treatment for cancer for more than 100 years, with its earliest roots traced from the discovery of X-rays in 1895 by Wilhelm Röntgen.
[120] The field of radiation therapy began to grow in the early 1900s largely due to the groundbreaking work of Nobel Prize–winning scientist Marie Curie (1867–1934), who discovered the radioactive elements polonium and radium in 1898.
CT-based planning allows physicians to more accurately determine the dose distribution using axial tomographic images of the patient's anatomy.
These advances allowed radiation oncologists to better see and target tumors, which have resulted in better treatment outcomes, more organ preservation and fewer side effects.


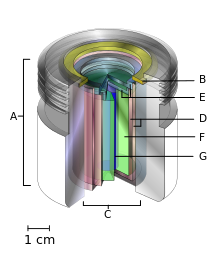
- an international standard source holder (usually lead),
- a retaining ring, and
- a teletherapy "source" composed of
- two nested stainless steel canisters welded to
- two stainless steel lids surrounding
- a protective internal shield (usually uranium metal or a tungsten alloy) and
- a cylinder of radioactive source material, often but not always cobalt-60 . The diameter of the "source" is 30 mm.


