Rectal prolapse
[5] It describes ulceration of the rectal lining caused by repeated frictional damage as the internal intussusception is forced into the anal canal during straining.
This classification also takes into account sphincter relaxation:[19] Rectal internal mucosal prolapse has been graded according to the level of descent of the intussusceptum, which was predictive of symptom severity:[20] The most widely used classification of internal rectal prolapse is according to the height on the rectal/sigmoid wall from which they originate and by whether the intussusceptum remains within the rectum or extends into the anal canal.
[10] It may be used to assess for pelvic floor dyssenergia,[5] (anismus is a contraindication for certain surgeries, e.g. STARR), and these patients may benefit from post-operative biofeedback therapy.
[21] When males are affected, they tend to be young and report significant bowel function symptoms, especially obstructed defecation,[5] or have a predisposing disorder (e.g., congenital anal atresia).
Shortly after the invention of defecography, In 1968 Broden and Snellman used cinedefecography to show that rectal prolapse begins as a circumferential intussusception of the rectum,[3][10] which slowly increases over time.
[21] This proved an older theory from the 18th century by John Hunter and Albrecht von Haller that this condition is essentially a full-thickness rectal intussusception, beginning about 3 inches above the dentate line and protruding externally.
[9] This excessive straining may be due to predisposing pelvic floor dysfunction (e.g. obstructed defecation) and anatomical factors:[10][21] Some authors question whether these abnormalities are the cause, or secondary to the prolapse.
[5] The assumed mechanism of obstructed defecation is by disruption to the rectum and anal canal's ability to contract and fully evacuate rectal contents.
[30] The factors that result in a patient progressing from internal intussusception to a full thickness rectal prolapse remain unknown.
[5] Defecography studies demonstrated that degrees of internal intussusception are present in 40% of asymptomatic subjects, raising the possibility that it represents a normal variant in some, and may predispose patients to develop symptoms, or exacerbate other problems.
[10] Alternatively, perineal procedures may be selected to reduce risk of nerve damage, for example in young male patients for whom sexual dysfunction may be a major concern.
Redundant rectal and sigmoid wall is removed and the new edge of colon is reconnected (anastomosed) with the anal canal with stitches or staples.
[3] Delorme Procedure This is a modification of the perineal rectosigmoidectomy, differing in that only the mucosa and submucosa are excised from the prolapsed segment, rather than full thickness resection.
"Mucosal proctectomy" was first discussed by Delorme in 1900,[10] now it is becoming more popular again as it has low morbidity and avoids an abdominal incision, while effectively repairing the prolapse.
Complications, including infection, urinary retention, bleeding, anastomotic dehiscence (opening of the stitched edges inside), rectal stricture (narrowing of the gut lumen), diarrhea, and fecal impaction occur in 6-32% of cases.
[5] Degrees of internal intussusception have been demonstrated in 40% of asymptomatic subjects, raising the possibility that it represents a normal variant in some, and may predispose patients to develop symptoms, or exacerbate other problems.
[11] It has been observed that intussusceptions of thickness ≥3 mm, and those that appear to cause obstruction to rectal evacuation may give clinical symptoms.
[43] One study concluded that intussusception of the anterior rectal wall shares the same cause as rectocele, namely deficient recto-vaginal ligamentous support.
[5] Nonsurgical measures to treat internal intussusception include pelvic floor retraining,[48] a bulking agent (e.g. psyllium), suppositories or enemas to relieve constipation and straining.
[49] Some researchers advise that internal intussusception be managed conservatively, compared to external rectal prolapse which usually requires surgery.
Generally, a section of rectal wall can be resected (removed), or the rectum can be fixed (rectopexy) to its original position against the sacral vertebrae, or a combination of both methods.
[54] Complications include constipation, which is reduced if the technique does not use posterior rectal mobilization (freeing the rectum from its attached back surface).
[60] STARR is contraindicated in patients with weak sphincters (fecal incontinence and urgency are a possible complication) and with anismus (paradoxical contraction of the pelvic floor during attempted defecation).
Symptom severity increases with the size of the prolapse, and whether it spontaneously reduces after defecation, requires manual reduction by the patient, or becomes irreducible.
Solitary rectal ulcer syndrome (SRUS, SRU), is a disorder of the rectum and anal canal, caused by straining and increased pressure during defecation.
[68] Pathological specimens of sections of rectal wall taken from SRUS patients show thickening and replacement of muscle with fibrous tissue and excess collagen.
Cystica profunda is characterized by formation of mucin cysts in the muscle layers of the gut lining, and it can occur anywhere along the gastrointestinal tract.
Stopping straining during bowel movements, by use of correct posture, dietary fiber intake (possibly included bulk forming laxatives such as psyllium), stool softeners (e.g. polyethylene glycol,[85][86] and biofeedback retraining to coordinate pelvic floor during defecation.
Michelle Lhooq, writing for VICE, argues that rosebudding is an example of producers making 'extreme' content due to the easy availability of free pornography on the internet.
[92] Repeated rectal prolapses can cause bowel problems and anal leakage and therefore risk the health of pornographic actors or actresses who participate in them.
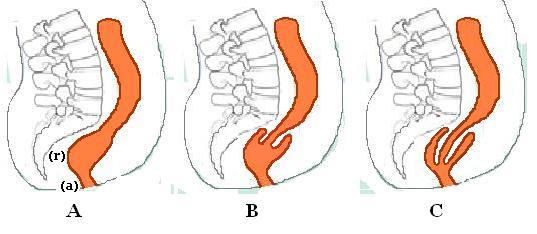
B. Recto-rectal intussusception
C. Recto-anal intussusception

