Renal ultrasonography
Furthermore, novel applications in renal US have been introduced with contrast-enhanced ultrasound (CEUS), elastography and fusion imaging.
In the normal kidney, the urinary collecting system in the renal sinus is not visible, but it creates a heteroechoic appearance with the interposed fat and vessels.
The parenchyma is more hypoechoic and homogenous and is divided into the outermost cortex and the innermost and slightly less echogenic medullary pyramids.
In the pediatric patient, it is easier to differentiate the hypoechoic medullar pyramids from the more echogenic peripheral zone of the cortex in the parenchyma rim, as well as the columns of Bertin (Figure 2).
In neonates and children up to six months of age, the cortex is more echogenic than the liver and spleen when compared at the same depth.
[1] Complex cysts can have membranes dividing the fluid-filled center with internal echoes, calcifications or irregular thickened walls.
[1] In polycystic kidney disease, multiple cysts of varying size in close contact with each other are seen filling virtually the entire renal region.
RCCs are typically isoechoic and peripherally located in the parenchyma, but can be both hypo- and hyper-echoic and are found centrally in medulla or sinus.
RCC is associated with von Hippel–Lindau disease, and with tuberous sclerosis, and US has been recommended as a tool for assessment and follow-up of renal masses in these patients.
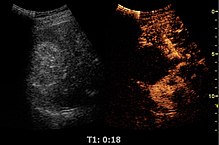
In RCCs, Doppler US often shows vessels with high velocities caused by neovascularization and arteriovenous shunting.
In special cases of cystic or solid renal masses, additional US guided biopsy or drainage is performed to identify the histologic tumor type before a decision on surgery is made.
In children, hydronephrosis can be caused by ureteropelvic junction obstruction, ectopic inserted ureter, primary megaureter and posterior urethral valve (Figure 13).
The evaluation of hydronephrosis can also include measures of calyces at the level of the neck in the longitudinal scan plane, of the dilated renal pelvis in the transverse scan plane and the cortical thickness, as explained previously (Figure 16 and Figure 17).
[1] If the fluid in the dilated collecting system has echoes, pyonephrosis should be excluded by clinical exam, blood analysis and, in special cases, puncture or drainage.
Hydronephrosis can also be caused by non-obstructive conditions, such as brisk diuresis in patients treated with diuretics, in pregnant women and in children with vesicoureteral reflux.
Whether the underlying pathologic change is glomerular sclerosis, tubular atrophy, interstitial fibrosis or inflammation, the result is often increased echogenicity of the cortex.
CT is preferred in renal traumas, but US is used for follow-up, especially in the patients suspected for the formation of urinomas (Figure 28).
Historically, thermal ablation of renal tumors is performed under CT guidance, as the risk of injuring neighboring intestines during the US-guided procedure was considered too high due to poor identification of the moving bowels.
However, recent guidelines for renal interventional US include radiofrequency, microwave and cryoablation with US as the ideal imaging guide.
However, CEUS is used in some patients after ablation of renal cell carcinoma to evaluate contrast uptake in the treated area (Figure 30).
Image fusion of ultrasound with a previously recorded dataset of CT or other modalities is rarely used in renal US.
Preliminary reports on US elastography used on transplanted kidneys to evaluate cortical fibrosis have been published showing promising results (Figure 32).