Schizophrenia
Schizophrenia is a mental disorder[17][7] characterized variously by hallucinations (typically, hearing voices), delusions, disorganized thinking and behavior,[10] and flat or inappropriate affect.
[21] Possible environmental factors include being raised in a city, childhood adversity, cannabis use during adolescence, infections, the age of a person's mother or father, and poor nutrition during pregnancy.
[25][26] Compared to the general population, people with schizophrenia have a higher suicide rate (about 5% overall) and more physical health problems,[27][28] leading to an average decrease in life expectancy by 20[13] to 28 years.
[55] Neurocognition is the ability to receive and remember information, and includes verbal fluency, memory, reasoning, problem solving, speed of processing, and auditory and visual perception.
[60] Neurological soft signs of clumsiness and loss of fine motor movement are often found in schizophrenia, which may resolve with effective treatment of FEP.
[61][78] Schizophrenia is described as a neurodevelopmental disorder with no precise boundary, or single cause, and is thought to develop from gene–environment interactions with involved vulnerability factors.
Response to stress can cause lasting changes in the function of the HPA axis possibly disrupting the negative feedback mechanism, homeostasis, and the regulation of emotion leading to altered behaviors.
A number of potential explanations have been proposed, including that alleles associated with schizophrenia risk confers a fitness advantage in unaffected individuals.
[27] The prevailing model of schizophrenia is that of a neurodevelopmental disorder, and the underlying changes that occur before symptoms become evident are seen as arising from the interaction between genes and the environment.
[77] Maternal infections, malnutrition and complications during pregnancy and childbirth are known risk factors for the development of schizophrenia, which usually emerges between the ages of 18 and 25, a period that overlaps with certain stages of neurodevelopment.
[128] The most common model put forward was the dopamine hypothesis of schizophrenia, which attributes psychosis to the mind's faulty interpretation of the misfiring of dopaminergic neurons.
Astrocytes are crucial in contributing to the formation and maintenance of neural circuits and it is believed that disruption in this role can result in a number of neurodevelopmental disorders including schizophrenia.
Although these functions are separable, their dysfunction in schizophrenia may reflect an underlying deficit in the ability to represent goal related information in working memory, and to use this to direct cognition and behavior.
For example, functional neuroimaging studies report evidence of reduced neural processing efficiency, whereby the dorsolateral prefrontal cortex is activated to a greater degree to achieve a certain level of performance relative to controls on working memory tasks.
These cellular and functional abnormalities may also be reflected in structural neuroimaging studies that find reduced grey matter volume in association with deficits in working memory tasks.
However, a large body of evidence suggests that hedonic responses are intact in schizophrenia,[150] and that what is reported to be anhedonia is a reflection of dysfunction in other processes related to reward.
In approved models of circuits that mediate predictive coding, reduced NMDA receptor activation, could in theory result in the positive symptoms of delusions and hallucinations.
[195][29] Clozapine is of benefit to around half of this group although it has the potentially serious side effect of agranulocytosis (lowered white blood cell count) in less than 4% of people.
This approach is known as assertive community treatment (ACT) and has been shown to achieve positive results in symptoms, social functioning and quality of life.
[215][216] However, other studies have found that CBT does improve overall psychotic symptoms (when in use with medication) and it has been recommended in Canada, but has been seen to have no effect on social function, relapse, or quality of life.
[14] This is primarily because of its association with heart disease,[230] diabetes,[14] obesity, poor diet, a sedentary lifestyle, and smoking, with an increased rate of suicide playing a lesser role.
[233] Barriers to improving the mortality rate in schizophrenia are poverty, overlooking the symptoms of other illnesses, stress, stigma, and medication side effects.
[251][252] Poor cognitive functioning, decision-making, and facial perception may contribute to making a wrong judgement of a situation that could result in an inappropriate response such as violence.
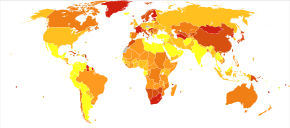
[56] The frequency of schizophrenia varies across the world,[10] within countries,[257] and at the local and neighborhood level;[258] this variation in prevalence between studies over time, across geographical locations, and by gender is as high as fivefold.
In 1893 Emil Kraepelin used the term in making a distinction, known as the Kraepelinian dichotomy, between the two psychoses: dementia praecox and manic depression (now called bipolar disorder).
[280] From the 1960s until 1989, psychiatrists in the USSR and Eastern Bloc diagnosed thousands of people with sluggish schizophrenia,[281][282] without signs of psychosis, based on "the assumption that symptoms would later appear".
[293] The book A Beautiful Mind chronicled the life of John Forbes Nash who had been diagnosed with schizophrenia and won the Nobel Memorial Prize in Economic Sciences.
[295][296] A 2015 Cochrane review found unclear evidence of benefit from brain stimulation techniques to treat the positive symptoms of schizophrenia, in particular auditory verbal hallucinations (AVHs).
Other inflammatory cytokines are found to be elevated in first episode psychosis and acute relapse that are normalized after treatment with antipsychotics, and these may be considered as state markers.
[302][303] Ongoing fMRI research aims to identify biomarkers within these brain networks,[304] potentially aiding in earlier diagnosis and better tracking of treatment responses in schizophrenia.





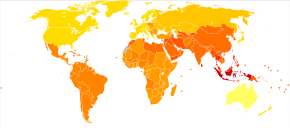
|
no data
≤ 185
185–197
197–207
207–218
218–229
229–240
|
240–251
251–262
262–273
273–284
284–295
≥ 295
|