Sinoatrial node
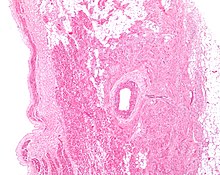
[3][4] The SA node is located in the wall (epicardium) of the right atrium, laterally to the entrance of the superior vena cava in a region called the sinus venarum (hence sino- + atrial).
The cells of the SA node are spread out within a mesh of connective tissue, containing nerves, blood vessels, collagen and fat.
[8] Action potentials pass from one cardiac cell to the next through pores known as gap junctions.
There are fewer gap junctions within the SA node and they are smaller in size.
Despite these many differences, there doesn't appear to be any advantage to how many sinoatrial nodal arteries an individual has, or where they originate.
This produces a positive change in membrane potential, known as depolarization, which is propagated throughout the heart and initiates muscle contraction.
[2] Other cells within the heart (including the Purkinje fibers[11] and atrioventricular node) can also initiate action potentials; however, they do so at a slower rate and therefore, if the SA node is functioning properly, its action potentials usually override those that would be produced by other tissues.
Immediately following repolarization, when the membrane potential is very negative (it is hyperpolarised), the voltage slowly begins to increase.
These channels allow a flow of Ca2+ into the cell, making the membrane potential even more positive.
[16] This is mainly due to the flow of Ca2+ through L-type calcium channels, which are now fully open.
This occurs due to the inactivation of L-type calcium channels (preventing the movement of Ca2+ into the cell) and the activation of potassium channels, which allows the flow of K+ out of the cell, making the membrane potential more negative.
Binding of NA to this receptor activates a G-protein (in particular a Gs-Protein, S for stimulatory) which initiates a series of reactions (known as the cAMP pathway) that results in the production of a molecule called cyclic adenosinemonophosphate (cAMP).
Binding of cAMP to the HCN increases the flow of Na+ and K+ into the cell, speeding up the pacemaker potential, so producing action potentials at a quicker rate and increasing heart rate.
The first cell to produce the action potential in the SA node isn't always the same; this is known as pacemaker shift.
[21] Blockage of the arterial blood supply to the SA node (most commonly due to a myocardial infarction or progressive coronary artery disease) can therefore cause ischemia and cell death in the SA node.
[22] The sinoatrial node was first discovered by a young medical student, Martin Flack, in the heart of a mole, whilst his mentor, Sir Arthur Keith, was on a bicycle ride with his wife.
They made the discovery in a makeshift laboratory set up in a farmhouse in Kent, England, called Mann's Place.