Spina bifida
[12] Occulta has no or only mild signs, which may include a hairy patch, dimple, dark spot or swelling on the back at the site of the gap in the spine.
[2] Problems associated with this form include poor ability to walk, impaired bladder or bowel control, accumulation of fluid in the brain, a tethered spinal cord and latex allergy.
[2] Some experts believe such an allergy can be caused by frequent exposure to latex, which is common for people with spina bifida who have shunts and have had many surgeries.
[5] Before birth, if a blood test or amniocentesis finds a high level of alpha-fetoprotein (AFP), there is a higher risk of spina bifida.
[21] A systematic review of radiographic research studies found no relationship between spina bifida occulta and back pain.
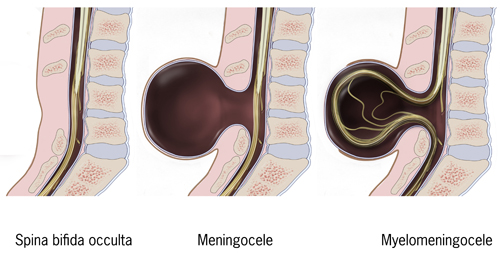
As the nervous system remains undamaged, individuals with meningocele are unlikely to have long-term health problems, although cases of tethered cord have been reported.
[citation needed] Myelomeningocele (MMC), also known as meningomyelocele, is the type of spina bifida that often results in the most severe complications and affects the meninges and nerves.
[35] The corpus callosum is abnormally developed in 70–90% of individuals with spina bifida myelomeningocele; this affects the communication processes between the left and right brain hemispheres.
[43] Unlike typically developing children, youths with spina bifida do not tend to improve in their executive functioning as they grow older.
[47] In addition to brain abnormalities directly related to various academic skills, achievement is likely affected by impaired attentional control and executive functioning.
[48] Individuals with spina bifida have demonstrated stable difficulties with arithmetic accuracy and speed, mathematical problem-solving, and general use and understanding of numbers in everyday life.
[53] Individuals with spina bifida may have difficulty with writing due to deficits in fine motor control and working memory.
[citation needed] Research has shown the lack of folic acid (folate) is a contributing factor in the pathogenesis of neural tube defects, including spina bifida.
Folate supplementation prior to conception has been found to reduce the risk of neural tube defects, including spina bifida, by 70%.
[59] Sources of folic acid include whole grains, fortified breakfast cereals, dried beans, leaf vegetables and fruits.
[67] The U.S. Food and Drug Administration, Public Health Agency of Canada[68] and the UK Department of Health and Social Care (DHSC) recommended amount of folic acid for women of childbearing age and women planning to become pregnant is at least 0.4 mg/day of folic acid from at least three months before conception, and continued for the first 12 weeks of pregnancy.
[citation needed] Risks of amniocentesis, which may occur in approximately 1 in 900 tests, include leaking amniotic fluid, though this generally has no effect on pregnancy.
Ultrasound screening for spina bifida is partly responsible for the decline in new cases, because many pregnancies are terminated out of fear that a newborn might have a poor future quality of life.
In addition, a shunt may be surgically installed to provide a continuous drain for the excess cerebrospinal fluid produced in the brain, as happens with hydrocephalus.
Healthcare professionals working with adults may also be less knowledgeable about spina bifida because it is considered a childhood chronic health condition.
[80] An increased dependence on others (in particular family members) may interfere with the adolescent's self-management of health-related tasks, such as catheterization, bowel management, and taking medications.
[81] As part of the transition process, it is beneficial to begin discussions at an early age about educational and vocational goals, independent living, and community involvement.
[82] Certain locations feature multidisciplinary clinics in order to offer coordinated care between specialists, such as Cincinnati Children's Center for Spina Bifida.
[84][85] Since then, the rate has fallen dramatically with 0.15 per 1000 live births reported in 1998,[58] though this decline is partially accounted for because some fetuses are aborted when tests show signs of spina bifida (see Pregnancy screening above).
Although Hippocratic doctors were aware of developmental abnormalities involving the lower spine, the first person to describe a spinal spina bifida was a Persian physician Al-Razi (Rhazes, 865–925 AD).
[90] Surgeons at Vanderbilt University, led by Joseph Bruner, attempted to close spina bifida in 4 human fetuses using a skin graft from the mother using a laparoscope.
[98][99] The trial concluded that the outcomes after prenatal spina bifida treatment are improved to the degree that the benefits of the surgery outweigh the maternal risks.
[104] The observations in mothers and their fetuses that were operated over the past two and a half years by the matured minimally invasive approach showed the following results: Compared to the open fetal surgery technique, fetoscopic repair of myelomeningocele results in far less surgical trauma to the mother, as large incisions of her abdomen and uterus are not required.
As a result, thinning of the uterine wall or dehiscence which have been among the most worrisome and criticized complications after the open operative approach do not occur following minimally invasive fetoscopic closure of spina bifida aperta.
The current cost of the entire fetoscopic procedure, including hospital stay, drugs, perioperative clinical, ECG, ultrasound and MRI-examinations, is approximately €16,000.