T cell
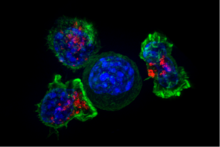
Groups of specific, differentiated T cell subtypes have a variety of important functions in controlling and shaping the immune response.
The specific adaptive immune response regulated by the TH cell depends on its subtype (such as T-helper1, T-helper2, T-helper17, regulatory T-cell),[4] which is distinguished by the types of cytokines they secrete.
Each mature T cell will ultimately contain a unique TCR that reacts to a random pattern, allowing the immune system to recognize many different types of pathogens.
These cells then undergo a round of proliferation, and begin to re-arrange the TCRα locus during the double-positive stage.
[12] mTECs must be Autoimmune regulator positive (AIRE+) to properly express tissue-specific antigens on their MHC class I peptides.
[13] This process is an important component of central tolerance and serves to prevent the formation of self-reactive T cells that are capable of inducing autoimmune diseases in the host.
Next, positive selection checks that thymocytes have successfully rearranged their TCRα locus and are capable of recognizing MHC molecules with appropriate affinity.
Negative selection in the medulla then eliminates thymocytes that bind too strongly to self-antigens expressed on MHC molecules.
Typical naive T cells that leave the thymus (via the corticomedullary junction) are self-restricted, self-tolerant, and single positive.
Mutations of the FOXP3 gene can prevent regulatory T cell development, causing the fatal autoimmune disease IPEX.
[32][33] In humans, MAIT cells are found in the blood, liver, lungs, and mucosa, defending against microbial activity and infection.
[32] The MHC class I-like protein, MR1, is responsible for presenting bacterially-produced vitamin B metabolites to MAIT cells.
[36] In addition to possessing innate-like functions, this T cell subset supports the adaptive immune response and has a memory-like phenotype.
However, γδ T cells are not MHC-restricted and seem to be able to recognize whole proteins rather than requiring peptides to be presented by MHC molecules on APCs.
Many microbes produce the active compound hydroxy-DMAPP (HMB-PP) and corresponding mononucleotide conjugates, in addition to IPP and DMAPP.
Both are required for production of an effective immune response; in the absence of co-stimulation, T cell receptor signalling alone results in anergy.
[45][46][47] The first signal is provided by binding of the T cell receptor to its cognate peptide presented on MHCII on an APC.
PLC-γ cleaves PI(4,5)P2 on the inner leaflet of the membrane to create the active intermediaries diacylglycerol (DAG), inositol-1,4,5-trisphosphate (IP3); PI3K also acts on PIP2, phosphorylating it to produce phosphatidlyinositol-3,4,5-trisphosphate (PIP3).
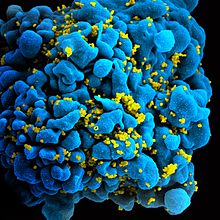
Complete insufficiency of T cell function can result from hereditary conditions such as severe combined immunodeficiency (SCID), Omenn syndrome, and cartilage–hair hypoplasia.
[60] "The first approach primarily defines as exhausted the cells that present the same cellular dysfunction (typically, the absence of an expected effector response).
The second approach primarily defines as exhausted the cells that are produced by a given cause (typically, but not necessarily, chronic exposure to an antigen).
"[60] Dysfunctional T cells are characterized by progressive loss of function, changes in transcriptional profiles and sustained expression of inhibitory receptors.
At first, cells lose their ability to produce IL-2 and TNFα, which is followed by the loss of high proliferative capacity and cytotoxic potential, and eventually leads to their deletion.
Exhausted T cells typically indicate higher levels of CD43, CD69 and inhibitory receptors combined with lower expression of CD62L and CD127.
Later after the initial septic encounter anti-inflammatory cytokines and pro-apoptotic proteins take over to protect the body from damage.
[74][75][76] While during infection T cell exhaustion can develop following persistent antigen exposure after graft transplant similar situation arises with alloantigen presence.
[73][79] Several studies showed positive effect of chronic infection on graft acceptance and its long-term survival mediated partly by T cell exhaustion.
[83] While there are data showing that induction of T cell exhaustion can be beneficial for transplantation it also carries disadvantages among which can be counted increased number of infections and the risk of tumor development.
[88] Some studies have suggested that it is possible to predict relapse of leukemia based on expression of inhibitory receptors PD-1 and TIM-3 by T cells.
[90] Inhibitory receptors targeted by those medical procedures are vital in T cell exhaustion and blocking them can reverse these changes.