Breast reconstruction
Generally, the aesthetic appearance is acceptable to the woman, but the reconstructed area is commonly completely numb afterwards, which results in loss of sexual function as well as the ability to perceive pain caused by burns and other injuries.
Originally, delayed reconstruction was believed to provide patients with time to psychologically adjust to the mastectomy and its effects on body image.
[2] As with many other surgeries, patients with significant medical comorbidities (e.g., high blood pressure, obesity, diabetes) and smokers are higher-risk candidates.
Implant-based reconstruction is an option for patients who have sufficient skin after mastectomy to cover a prosthetic implant and allow for a natural shape.
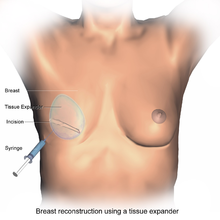
During two-stage reconstruction, the surgeon will insert a tissue expander underneath the pectoralis major muscle of the chest wall at the time of mastectomy.
[3] Following this initial procedure, the patient must return to the clinic on multiple occasions for saline to be injected into a tube inside the tissue expander.
By doing this slowly over the course of several weeks, the space beneath the pectoralis major muscle is safely expanded to an appropriate size without causing too much stress on the breast tissue.
[3] The sub-pectoral technique described above is now preferred because it provides an additional muscular layer between the skin and the implant, decreasing the risk of visible deformity.
If this is the case, one option is to use an acellular dermal matrix to cover the exposed portion of the prosthetic implant, improving both functional and aesthetic outcomes.
[9][10] This prepectoral space has recently, however, come back into practice, with comparable rates of post-operative complications and implant loss to submuscular placement.
[13] Of note, a Cochrane review published in 2016 concluded that implants for use in breast reconstructive surgery have not been adequately studied in good quality clinical trials.
The latissimus dorsi flap has a number of advantages, but despite the advances in surgical techniques, it has remained vulnerable to skin dehiscence or necrosis at the donor site (on the back).
That said, TRAM flap procedures can potentially weaken the abdominal wall and torso strength, but they are generally well tolerated by most patients.
Other donor sites for autologous breast reconstruction include the buttocks, which provides tissue for the SGAP and IGAP (superior and inferior gluteal artery perforator, respectively) flaps.
[20] The purpose of perforator flaps (DIEP, SIEA, SGAP, IGAP) is to provide sufficient skin and fat for an aesthetic reconstruction while minimizing post-operative complications from harvesting the underlying muscles.
By using a laser and 3D printer, a patient-specific silicone mold can be used as an aid during surgery, used as a guide for orienting and shaping the flap to improve accuracy and symmetry.
The transverse rectus abdominis myocutaneous (TRAM) flap method results in weakness and loss of flexibility in the abdominal wall.
[27] Outcomes-based research on quality of life improvements and psychosocial benefits associated with breast reconstruction [30][31] served as the stimulus in the United States for the 1998 Women's Health and Cancer Rights Act, which mandated that health care payer cover breast and nipple reconstruction, contralateral procedures to achieve symmetry, and treatment for the sequelae of mastectomy.