Transverse myelitis
The spinal cord inflammation seen in TM has been associated with various infections, immune system disorders, or damage to nerve fibers, by loss of myelin.
Motor weakness occurs due to the involvement of the pyramidal tracts and mainly affects the muscles that flex the legs and extend the arms.
[5] A lesion of the thoracic segment (T1–12) will produce upper motor neuron signs in the lower limbs, presenting as a spastic paraparesis.
Lyme disease gives rise to neuroborreliosis which is seen in a small percentage (4 to 5 per cent) of acute transverse myelitis cases.
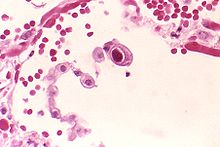
[16][17] This progressive loss of the fatty myelin sheath surrounding the nerves in the affected spinal cord occurs for unclear reasons following infections or due to multiple sclerosis.
[4] A proposed special clinical presentation is the "longitudinally extensive transverse myelitis" (LETM), which is defined as a TM with a spinal cord lesion that extends over three or more vertebral segments.
If breathing is affected, particularly in upper spinal cord lesions, methods of artificial ventilation must be on hand before and during the transfer procedure.
Corticosteroids are often given in high doses when symptoms begin with the hope that the degree of inflammation and swelling of the spinal cord will be lessened, but whether this is truly effective is still debated.
[25] The earliest reports describing the signs and symptoms of transverse myelitis were published in 1882 and 1910 by the English neurologist Henry Bastian.
His suggestion was consistent with reports in 1922 and 1923 of rare instances in which patients developed "post-vaccinal encephalomyelitis" subsequent to receiving the rabies vaccine which then was made from brain tissue carrying the virus.
The pathological examination of those who had died from the disease revealed inflammatory cells and demyelination as opposed to the vascular lesions predicted by Bastian.
[29] In 1948, Dr. Suchett-Kaye described a patient with rapidly progressing impairment of lower extremity motor function that developed as a complication of pneumonia.
In his description, he coined the term transverse myelitis to reflect the band-like thoracic area of altered sensation that patients reported.
Bastian's initial description included few conclusive diagnostic criteria; by the 1980s, basic diagnostic criteria were established, including acutely developing paraparesis combined with bilateral spinal cord dysfunction for <4 weeks and a well-defined upper sensory level, no evidence of spinal cord compression, and a stable, non-progressive course.
[31][32] Later definitions, were written to exclude patients with underlying systemic or neurological illnesses and to include only those who progressed to maximum deficit in fewer than 4 weeks.
The word is from Latin: myelitis transversa and the disorder's name is derived from Greek myelós referring to the "spinal cord", and the suffix -itis, which denotes inflammation.