Medical ultrasound
[10] Superficial structures such as muscle, tendon, testis, breast, thyroid and parathyroid glands, and the neonatal brain are imaged at higher frequencies (7–18 MHz), which provide better linear (axial) and horizontal (lateral) resolution.
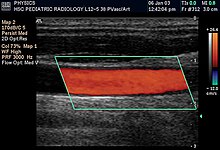
[citation needed] In angiology or vascular medicine, duplex ultrasound (B Mode imaging combined with Doppler flow measurement) is used to diagnose arterial and venous disease.
[citation needed] Echocardiography is an essential tool in cardiology, assisting in evaluation of heart valve function, such as stenosis or insufficiency, strength of cardiac muscle contraction, and hypertrophy or dilatation of the main chambers.
In abdominal sonography, the major organs of the abdomen such as the pancreas, aorta, inferior vena cava, liver, gall bladder, bile ducts, kidneys, and spleen may be imaged.
[14][15] Gynecologic ultrasonography examines female pelvic organs (specifically the uterus, ovaries, and fallopian tubes) as well as the bladder, adnexa, and pouch of Douglas.
[citation needed] In neonatology, transcranial Doppler can be used for basic assessment of intracerebral structural abnormalities, suspected hemorrhage, ventriculomegaly or hydrocephalus and anoxic insults (periventricular leukomalacia).
It can be performed through the soft spots in the skull of a newborn infant (Fontanelle) until these completely close at about 1 year of age by which time they have formed a virtually impenetrable acoustic barrier to ultrasound.
This imaging modality is used at the bedside or examination table to evaluate a number of different lung abnormalities as well as to guide procedures such as thoracentesis, (drainage of pleural fluid (effusion)), needle aspiration biopsy, and catheter placement.
[61] Uses include: A contrast medium for medical ultrasonography is a formulation of encapsulated gaseous microbubbles[64] to increase echogenicity of blood, discovered by Dr. Raymond Gramiak in 1968[65] and named contrast-enhanced ultrasound.
[67] Other clinical applications using contrast exist, as in echocardiography to improve delineation of left ventricle for visualizing contractibility of heart muscle after a myocardial infarction.
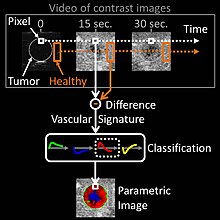
Finally, applications in quantitative perfusion[68] (relative measurement of blood flow[69]) have emerged for identifying early patient response to anti-cancerous drug treatment (methodology and clinical study by Dr. Nathalie Lassau in 2011[70]), enabling the best oncological therapeutic options to be determined.
This method is based on medical computational science[74][75] to analyze a time sequence of ultrasound contrast images, a digital video recorded in real-time during patient examination.
This parametric image is interpreted by clinicians based on predominant colorization of the tumor: red indicates a suspicion of malignancy (risk of cancer), green or yellow – a high probability of benignity.
The main clinical benefits are to avoid a systemic biopsy (with inherent risks of invasive procedures) of benign tumors or a CT scan examination exposing the patient to X-ray radiation.
The current future of contrast ultrasonography is in molecular imaging with potential clinical applications expected in cancer screening to detect malignant tumors at their earliest stage of appearance.
As a result, a few minutes after their injection in blood circulation, the targeted microbubbles accumulate in the malignant tumor; facilitating its localization in a unique ultrasound contrast image.
[84] In molecular ultrasonography, the technique of acoustic radiation force (also used for shear wave elastography) is applied in order to literally push the targeted microbubbles towards microvessels wall; first demonstrated by Dr. Paul Dayton in 1999.
At the stage of scientific preclinical research, the technique of acoustic radiation force was implemented as a prototype in clinical ultrasound systems and validated in vivo in 2D[86] and 3D[87][88] imaging modes.
For example, one study combined B-mode, colour Doppler, real-time elastography, and contrast-enhanced ultrasound, achieving an accuracy similar to that of multiparametric MRI.
The FDA requires that the machine not exceed established limits, which are reasonably conservative in an effort to maintain diagnostic ultrasound as a safe imaging modality.
With concerns about its misuse for sex-selective abortion, the Government of India passed the Pre-natal Diagnostic Techniques Act (PNDT) in 1994 to distinguish and regulate legal and illegal uses of ultrasound equipment.
In 1940, the American acoustical physicist Floyd Firestone devised the first ultrasonic echo imaging device, the Supersonic Reflectoscope, to detect internal flaws in metal castings.
[129] Subsequent advances took place concurrently in several countries but it was not until 1961 that David Robinson and George Kossoff's work at the Australian Department of Health resulted in the first commercially practical water bath ultrasonic scanner.
[130] In 1963 Meyerdirk & Wright launched production of the first commercial, hand-held, articulated arm, compound contact B-mode scanner, which made ultrasound generally available for medical use.
[131] Donald was an obstetrician with a self-confessed "childish interest in machines, electronic and otherwise", who, having treated the wife of one of the company's directors, was invited to visit the Research Department of boilermakers Babcock & Wilcox at Renfrew.
These findings were reported in The Lancet on 7 June 1958[133] as "Investigation of Abdominal Masses by Pulsed Ultrasound" – possibly one of the most important papers published in the field of diagnostic medical imaging.
At GRMH, Professor Donald and James Willocks then refined their techniques to obstetric applications including fetal head measurement to assess the size and growth of the fetus.
Stuart Campbell's pioneering work on fetal cephalometry led to it acquiring long-term status as the definitive method of study of foetal growth.
Wright and Meyerdirk left the university to form Physionic Engineering Inc., which launched the first commercial hand-held articulated arm compound contact B-mode scanner in 1963.
Eventually, they developed technologies to use duplex imaging, or Doppler in conjunction with B-mode scanning, to view vascular structures in real time while also providing hemodynamic information.