Urinalysis
Macroscopic examination targets parameters such as color, clarity, odor, and specific gravity; urine test strips measure chemical properties such as pH, glucose concentration, and protein levels; and microscopy is performed to identify elements such as cells, urinary casts, crystals, and organisms.
The formation of urine takes place in microscopic structures called nephrons, about one million of which are found in a normal human kidney.
A healthy glomerulus allows many solutes in the blood to pass through, but does not permit the passage of cells or high-molecular weight substances such as most proteins.
[8] If the sample is not tested promptly, inaccurate results can occur because bacteria in the urine will multiply and elements such as cells and casts will degrade.
An unusually bright yellow color can occur after consumption of B vitamin supplements,[31] while phenazopyridine, used to treat urinary tract-related pain, can turn the urine orange.
[32] Phenolphthalein, a stimulant laxative previously found in Ex-Lax,[33] can produce colors ranging from red to purple, and levodopa, used to treat Parkinson's disease, may result in "cola-colored" urine.
[26] A milky appearance can be caused by a very high concentration of white blood cells or fats, or by chyluria (the presence of lymphatic fluid in the urine).
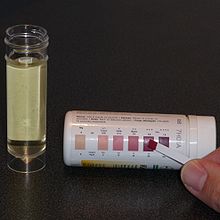
The strip is dipped into the urine sample and the color changes on the reagent pads are read after a defined period of time, either by eye or using an automated instrument.
[51] Red blood cells can sometimes be distinguished from free hemoglobin or myoglobin as the former causes a speckled pattern on the test pad while the latter results in a uniform color change.
[57][58] Not all bacteria that cause UTIs produce nitrite, and because it takes time for the chemical reaction to occur, the test is best performed on urine that has been in the bladder overnight.
[60][62] Conventional test strips are not sensitive enough to reliably detect microalbuminuria, a condition in which urine albumin levels are slightly elevated,[64] although dipsticks specialized for this measurement exist.
Urine pH varies with diet and a wide range of values occur in healthy subjects, although it is most commonly slightly acidic.
Because the kidneys are involved in regulating acid-base balance, the urine is typically acidic in people with metabolic or respiratory acidosis and alkaline in those with alkalosis.
When the body relies on fats, rather than carbohydrates, as its main energy source, increased levels of ketones occur in the blood and urine.
Conjugated bilirubin is normally stored in the gallbladder as a constituent of bile and is excreted through the intestines; it does not occur at detectable levels in the urine.
[85] Testing methods are based on the Ehrlich reaction of urobilinogen with para-dimethylaminobenzaldehyde, or interaction with a diazonium compound to produce a colored product.
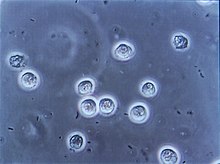
[92] If it is necessary to determine the exact number of cells or casts in the sample, unconcentrated urine can be placed in a counting chamber called a hemocytometer.
[93] Urine is traditionally examined by light microscopy, but some laboratories use phase-contrast microscopes, which improve the visualization of elements such as urinary casts and mucus.
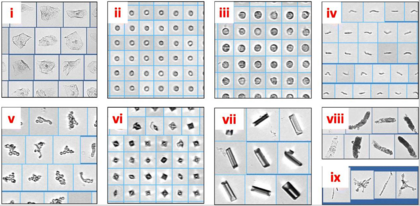
[94] Automated instruments reduce workload in medical laboratories and can accurately identify most common urinary elements, but do not perform as well with unusual findings such as transitional and renal epithelial cells, abnormal casts and rare crystals.
[107] In the absence of recent trauma to the urinary tract, clusters and sheets of transitional cells in the urine may indicate malignancy, requiring further investigation.
[138][140] When the dipstick test is positive, microscopy is used to confirm and count WBCs, RBCs and bacteria and assess for possible contamination (signified by a high number of squamous epithelial cells in the sample).
[139] If UTI is suspected, particularly in complicated cases or when urinalysis results are inconclusive,[140] a urine culture may be performed to identify microorganisms if present, obtain a colony count, and carry out antibiotic sensitivity testing.
[97] Hemoglobinuria, if unaccompanied by a high quantity of RBCs, can signify intravascular hemolysis (destruction of red blood cells inside the body).
[146] The causes of macroscopic hematuria are similar, but in the absence of an obvious explanation such as trauma or UTI, it is more strongly associated with malignancy and requires further investigation.
The 7th-century manuscript De Urinis by the Byzantine physician Theophilus Protospatharius is thought to be the earliest publication dedicated solely to the examination of urine.
Publications by Isaac Judaeus built upon Protospatharius' work, and Zayn al-Din Gorgani, an 11th-century Persian physician, published instructions for specimen collection which noted that urine samples were affected by aging and exposure to heat and light.
"Uromancers" without medical training claimed that they could not only diagnose disease, but detect pregnancy, determine a baby's sex, and even predict the future from a subject's urine.
In 1637 the English physician Thomas Brian published The Pisse-Prophet, or, Certaine Pisse-Pot Lectures, excoriating those who claimed to be able to diagnose diseases by uroscopy without examining the patient.
[161][162] The 19th century saw a proliferation in chemical methods for the analysis of urine, but these techniques were labor-intensive and impractical; in one contemporary editorial a physician complained about the dangers of keeping nitric acid (used to detect albumin) in one's pocket.
In the 1880s William Pavy developed powdered reagents for urinalysis, and George Oliver introduced "Urinary Test Papers" for albumin and glucose, which were a commercial success and were marketed in Germany as well as the United Kingdom.