Vein
[3] In medium and large sized veins the flow of blood is maintained by one-way (unidirectional) venous valves to prevent backflow.
[5][page needed] Veins close to the surface of the skin appear blue for a variety of reasons.
A subcutaneous venous plexus is continuous, and a high rate of flow is supplied by small arteriovenous anastomoses.
[20] The venous valves serve to prevent regurgitation (backflow) due to the low pressure of veins, and the pull of gravity.
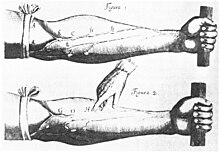
[20][21] A venous valve is bicuspid (having two leaflets) and is formed by an infolding of part of the tunica intima on either side of the lumen of the veins.
[22] When the blood tries to reverse its direction (due to low venous pressure and the pull of gravity), the sinuses fill first closing the leaflets and keeping them together.
[25] There are more valves in the lower leg, due to increased gravitational pull, with the number decreasing as the veins travel to the hip.
In the neck, the jugular veins parallel the upward course of the carotid arteries and drain blood into the superior vena cava.
This connection which is highly muscular, enables venous blood to travel directly from an artery into a vein without having passed from a capillary bed.
A small specialised arteriovenous anastomosis known as a glomus body or organ serves to transfer heat in the fingers and toes.
[14] A vascular shunt can also bypass the capillary bed and provide a route for blood supply directly to a collecting venule.
When all of the sphincters are closed blood can flow from a metarteriole into a thoroughfare channel and into a collecting venule bypassing the capillary bed.
[8] The middle tunica media is mainly of vascular smooth muscle cells, elastic fibers and collagen.
[30] Vascular smooth muscle cells control the size of the vein lumens, and thereby help to regulate blood pressure.
[31] The inner tunica intima is a lining of endothelium comprising a single layer of extremely flattened epithelial cells, supported by delicate connective tissue.
[4] The tunica intima has the most variation in blood vessels, in terms of their wall thickness and relative size of their lumen.
Veins have thinner walls than arteries, and a wider diameter that allow them to expand and hold a greater volume of blood.
Vascular smooth muscle cells control the size of the vein lumens, and thereby help to regulate blood pressure.
[31] The post-capillary venules are exchange vessels whose ultra-thin walls allow the ready diffusion of molecules from the capillaries.
Fainting can occur but usually baroreceptors within the aortic sinuses initiate a baroreflex such that angiotensin II and norepinephrine stimulate vasoconstriction and heart rate increases to return blood flow.
[38] The medical speciality involved with the diagnosis and treatment of venous disorders is known as phlebology (also venology), and the specialist concerned is a phlebologist.
[41] Immobility, active cancer, obesity, traumatic damage and congenital disorders that make clots more likely are all risk factors for deep vein thrombosis.
Intermittent pneumatic compression is a method used to improve venous circulation in cases of edema or in those at risk from a deep vein thrombosis.
SVT is not normally clinically significant, but the thrombus can migrate into the deep venous system where it can also give rise to a pulmonary embolism.
Other causes can include an obstructing clot in a hepatic vein (Budd Chiari syndrome) or compression from tumors or tuberculosis lesions.
[45] In a tumor such as infantile hemangioma the mass is soft, and easily compressed, and their coloring is due to the dilated anomalous involved veins.
He stated that "there must be small communications or pores (manafidh in Arabic) between the pulmonary artery and vein," a prediction that preceded the discovery of the capillary system by more than 400 years.
Finally, William Harvey, a pupil of Hieronymus Fabricius (who had earlier described the valves of the veins without recognizing their function), performed a sequence of experiments, and published Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus in 1628, which "demonstrated that there had to be a direct connection between the venous and arterial systems throughout the body, and not just the lungs.
Most importantly, he argued that the beat of the heart produced a continuous circulation of blood through minute connections at the extremities of the body.
However, Harvey was not able to identify the capillary system connecting arteries and veins; these were later discovered by Marcello Malpighi in 1661.