Diabetes medication
There are different classes of hypoglycemic drugs, and selection of the appropriate agent depends on the nature of diabetes, age, and situation of the person, as well as other patient factors.
Therapeutic combinations may include several insulin isoforms or varying classes of oral antihyperglycemic agents.
Insulins are typically characterized by the rate at which they are metabolized by the body, yielding different peak times and durations of action.
Although it must be used with caution in patients with impaired liver or kidney function, Metformin, a biguanide, has become the most commonly used agent for type 2 diabetes in children and teenagers.
[citation needed] Thiazolidinediones (TZDs), also known as "glitazones," bind to PPARγ, peroxisome proliferator activated receptor γ, a type of nuclear regulatory protein involved in the transcription of genes that regulate glucose and fat metabolism.
Some examples are: Multiple retrospective studies have resulted in a concern about rosiglitazone's safety, although it is established that the group, as a whole, has beneficial effects on diabetes.
The ADOPT study showed that initial therapy with drugs of this type may prevent the progression of disease,[18] as did the DREAM trial.
However, they are less preferred than GLP-1 agonists or SGLT2 inhibitors, especially in patients with cardiovascular disease (which liraglutide, empagliflozin, and canagliflozin are all FDA approved to treat).
The meta-analysis was not supported by an interim analysis of the trial designed to evaluate the issue, and several other reports have failed to conclude the controversy.
In contrast, at least one large prospective study, PROactive 05, has shown that pioglitazone may decrease the overall incidence of cardiac events in people with type 2 diabetes who have already had a heart attack.
[24] The LYN kinase activator Tolimidone has been reported to potentiate insulin signaling in a manner that is distinct from the glitazones.
[25] The compound has demonstrated positive results in a Phase 2a clinical study involving 130 diabetic subjects.
[citation needed] Current clinical practice guidelines from the AACE rate sulfonylureas (as well as glinides) below all other classes of antidiabetic drugs in terms of suggested use as first, second, or third line agents - this includes Bromocriptine, the bile acid sequestrant Colesevelam, α-glucosidase inhibitors, Thiazolidinediones (glitazones), and DPP-4 inhibitors (gliptins).
[20] The low cost of most sulfonylureas, however, especially when considering their significant efficacy in blood glucose reduction, tends to keep them as a more feasible option in many patients - neither SGLT2 inhibitors nor GLP-1 agonists, the classes most favored by the AACE guidelines after metformin, are currently available as generics.
Alpha-glucosidase inhibitors are a class of diabetes drugs found in plants/herbs like cinnamon;[3] however, they are technically not hypoglycemic agents because they do not have a direct effect on insulin secretion or sensitivity.
The intake of a single dose before a meal containing complex carbohydrates clearly suppresses the glucose spike and may decrease the postprandial hyperglycemia (higher than 140 mg/dL; >7.8 mmol/L) in patients with type II diabetes.
[27] These agents may also cause a decrease in gastric motility, responsible for the common side-effect of nausea, which tends to subside with time.
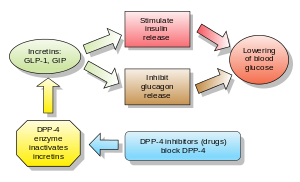
[27] GLP-1 analogs resulted in weight loss and had more gastrointestinal side-effects, while in general dipeptidyl peptidase-4 (DPP-4) inhibitors were weight-neutral and are associated with increased risk for infection and headache.
However, weight gain and/or hypoglycemia have been observed when dipeptidyl peptidase-4 inhibitors were used with sulfonylureas; effects on long-term health and morbidity rates are still unknown.
[44] A combined result of 5 RCTs enlisting a total of 279 patients aged 65 or older (mean baseline HbA1c of 8%) receiving 5 mg/d of saxagliptin was shown to reduce HbA1c by 0.73%.
[45] A combined result of 5 RCTs enlisting a total of 238 patients aged 65 or older (mean baseline HbA1c of 8.6%) receiving 100 mg/d of vildagliptin was shown to reduce HbA1c by 1.2%.
[46] Another set of 6 combined RCTs involving alogliptin (approved by FDA in 2013) was shown to reduce HbA1c by 0.73% in 455 patients aged 65 or older who received 12.5 or 25 mg/d of the medication.
The most frequent and severe adverse effect of pramlintide is nausea, which occurs mostly at the beginning of treatment and gradually reduces.
[50] Along with GLP-1 agonists, they are considered preferred second or third agents for type 2 diabetics sub-optimally controlled with metformin alone, according to most recent clinical practice guidelines.
Furthermore, there has been growing evidence that the effectiveness and safety of this drug class could depend on genetic variability of the patients.