Aortic stenosis
Aortic stenosis (AS or AoS) is the narrowing of the exit of the left ventricle of the heart (where the aorta begins), such that problems result.
[1] Signs of heart failure include shortness of breath especially when lying down, at night, or with exercise, and swelling of the legs.
[1] In those with severe disease a number of medications should be avoided, including ACE inhibitors, nitroglycerin, and some beta blockers.
Exercise stress testing with or without imaging is strictly contraindicated in symptomatic patients with severe aortic stenosis.
Exercise stress test is now recommended by current guidelines in asymptomatic patients and may provide incremental prognostic value.
At this point there may be signs of ventricular strain pattern (ST segment depression and T wave inversion) on the EKG, suggesting subendocardial ischemia.
Due to the hypertrophy of the left ventricle in aortic stenosis, including the consequent inability of the coronary arteries to adequately supply blood to the myocardium (see "Angina" below), abnormal heart rhythms may develop.
Notwithstanding the foregoing[clarification needed], the American Heart Association changed its recommendations regarding antibiotic prophylaxis for endocarditis.
Under normal circumstances, in the absence of aortic stenosis, the heart is able to increase its output and thereby offset the effect of the dilated blood vessels.
Degenerative (the most common variety), and bicuspid aortic stenosis both begin with damage to endothelial cells from increased mechanical stress.
Subsequently, fibroblasts differentiate into osteoblast-like cells, which results in abnormal bone matrix deposition leading to progressive valvular calcification and stenosis.
[26] As a consequence of this stenosis, the left ventricle must generate a higher pressure with each contraction to effectively move blood forward into the aorta.
In the later stages, the left ventricle dilates, the wall thins, and the systolic function deteriorates (resulting in impaired ability to pump blood forward).
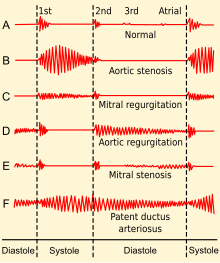
[4][12] The murmur increases with squatting and decreases with standing and isometric muscular contraction such as the Valsalva maneuver, which helps distinguish it from hypertrophic obstructive cardiomyopathy (HOCM).
[24] This is a result of the increasing calcification of the valve preventing it from "snapping" shut and producing a sharp, loud sound.
Due to increases in left ventricular pressure from the stenotic aortic valve, over time the ventricle may hypertrophy, resulting in diastolic dysfunction.
Hence, the physical exam in aortic stenosis may also reveal signs of the latter, for example, an early diastolic decrescendo murmur.
[31] Other peripheral signs include:[citation needed] For asymptomatic severe aortic valve stenosis, the European guidelines[35] recommend B-type natriuretic peptide (BNP) measurements to aid risk stratification and optimize the timing of aortic valve replacement surgery.
[7] Cardiac chamber catheterization provides a definitive diagnosis, indicating severe stenosis in valve area of <1.0 cm2 (normally about 3 cm2).
Cardiac catheterization is reserved for cases in which there is a discrepancy between the clinical picture and non-invasive testing, due to risks inherent to crossing the aortic valve, such as stroke.
A decreased valvular area causes increased pressure gradient, and these parameters are used to classify and grade the aortic stenosis as mild, moderate or severe.
[24] A chest X-ray can also assist in the diagnosis and provide clues as to the severity of the disease, showing the degree of calcification of the valve, and in a chronic condition, an enlarged left ventricle[12][24] and atrium.
[12] The use of CT calcium scoring is gaining spread as a diagnostic tool to complement echo in the assessment of patients with aortic stenosis.
[12] In moderate cases echocardiography is performed every 1–2 years to monitor the progression, possibly complemented with a cardiac stress test.
[24] In both moderate and mild cases, the person should immediately make a revisit or be admitted for inpatient care if any new related symptoms appear.
[48] Observational studies demonstrated an association between lowered cholesterol with statins and decreased progression, but a randomized clinical trial published in 2005 failed to find any effect on calcific aortic stenosis.
[7][49] In 2013 it was reported that trials did not show any benefit in slowing AS progression,[7] but did demonstrate a decrease in ischemic cardiovascular events.
[4] While Surgical AVR has remained the most effective treatment for this disease process and is currently recommended for patients after the onset of symptoms, as of 2016[update] aortic valve replacement approaches included open-heart surgery, minimally invasive cardiac surgery (MICS), and minimally invasive catheter-based (percutaneous) aortic valve replacement.
The surgeon will make a small incision at the top of the person's leg and proceed to insert the balloon into the artery.
[61] Acute decompensated heart failure due to AS may be temporarily managed by an intra-aortic balloon pump while pending surgery.