Barrett's esophagus
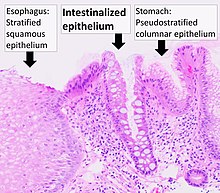
Barrett's esophagus is a condition in which there is an abnormal (metaplastic) change in the mucosal cells lining the lower portion of the esophagus, from stratified squamous epithelium to simple columnar epithelium with interspersed goblet cells that are normally present only in the small intestine and large intestine.
In this disease, acidic stomach, bile, and small intestine and pancreatic contents cause damage to the cells of the lower esophagus.
[11] This mechanism also explains the selection of HER2/neu (also called ERBB2) and the overexpressing (lineage-addicted) cancer cells during the process of carcinogenesis, and the efficacy of targeted therapy against the Her-2 receptor with trastuzumab (Herceptin) in the treatment of adenocarcinomas at the gastroesophageal junction.
The secretory columnar epithelium may be more able to withstand the erosive action of the gastric secretions; however, this metaplasia confers an increased risk of adenocarcinoma.
[citation needed] Since the COVID-19 pandemic In Scotland, the local NHS started using a swallowable sponge (Cytosponge) in hospitals to collect cell samples for diagnosis.
[18] Preliminary studies have shown this diagnostic test to be a useful tool for screening people with heartburn symptoms and improved diagnosis.
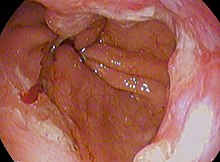
The metaplasia is grossly visible through a gastroscope, but biopsy specimens must be examined under a microscope to determine whether cells are gastric or colonic in nature.
The histochemical stain Alcian blue pH 2.5 is also frequently used to distinguish true intestinal-type mucins from their histologic mimics.
Recently, immunohistochemical analysis with antibodies to CDX-2 (specific for mid and hindgut intestinal derivation) has also been used to identify true intestinal-type metaplastic cells.
[26] After the initial diagnosis of Barrett's esophagus is rendered, affected persons undergo annual surveillance to detect changes that indicate higher risk to progression to cancer: development of epithelial dysplasia (or "intraepithelial neoplasia").
Although in the past physicians have taken a watchful waiting approach, newly published research supports consideration of intervention for Barrett's esophagus.
[33][34][35][36] The findings demonstrate radiofrequency ablation is at least 90% effective to completely clear Barrett's esophagus and dysplasia, with durability of up to five years and a favorable safety profile.
Laser treatment is used in severe dysplasia, while overt malignancy may require surgery, radiation therapy, or systemic chemotherapy.
A recent five-year random-controlled trial has shown that photodynamic therapy using photofrin is statistically more effective in eliminating dysplastic growth areas than sole use of a proton pump inhibitor.
[40] In a variety of studies, nonsteroidal anti-inflammatory drugs (NSAIDS) such as low-dose aspirin (75–300 mg/day) have shown evidence of preventing esophageal cancer in people with Barrett's esophagus.
[citation needed] A small subset of patients with Barrett's esophagus will eventually develop malignant esophagogastric junctional adenocarcinoma, which has a mortality rate of over 85%.
[46] This is partly due to each study having a different mix of intermediate disease states being combined under the umbrella diagnosis of LGD.
[55][56] In contrast, Philip Rowland Allison and Alan Johnstone argued that the condition related to the "esophagus lined with gastric mucous membrane and not intra-thoracic stomach as Barrett mistakenly believed.




adenocarcinoma (poor; signet-ringcell)