Complete blood count
The Coulter principle uses electrical impedance measurements to count blood cells and determine their sizes; it is a technology that remains in use in many automated analyzers.
[12][17] In emergency medicine, the CBC is used to investigate numerous symptoms, such as fever, abdominal pain, and shortness of breath,[18][19][20] and to assess bleeding and trauma.
[23] Regular CBCs are necessary for people taking some psychiatric drugs, such as clozapine and carbamazepine, which in rare cases can cause a life-threatening drop in the number of white blood cells (agranulocytosis).
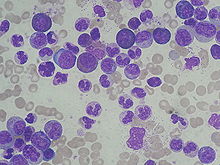
[29] The results of the CBC and smear examination reflect the functioning of the hematopoietic system—the organs and tissues involved in the production and development of blood cells, particularly the bone marrow.
Where laboratory facilities are not available, an estimate of hemoglobin concentration can be obtained by placing a drop of blood on a standardized type of absorbent paper and comparing it to a colour scale.
[99][100] For laboratories without access to commercial quality control material, an Indian regulatory organization recommends running patient samples in duplicate and comparing the results.
It is relatively stable over time compared to other CBC parameters, so a large change in MCV may indicate that the sample was drawn from the wrong patient.
[118] Based on the CBC results, further steps can be taken to investigate anemia, such as a ferritin test to confirm the presence of iron deficiency, or hemoglobin electrophoresis to diagnose a hemoglobinopathy such as thalassemia or sickle cell disease.
[136] A high white blood cell count, which is called leukocytosis, often occurs in infections, inflammation, and states of physiologic stress.
An increased number of band neutrophils—young neutrophils that lack segmented nuclei—or immature granulocytes is termed left shift and occurs in sepsis and some blood disorders, but is normal in pregnancy.
[159] It can occur in individuals who are undergoing treatments that suppress the bone marrow, such as chemotherapy or radiation therapy, or taking certain drugs, such as heparin, that can induce the immune system to destroy platelets.
[168] When people with nutritional anemia are given nutrient supplementation, an increase in the reticulocyte count indicates that their body is responding to the treatment by producing more red blood cells.
Some instruments measure the average amount of hemoglobin in each reticulocyte; a parameter that has been studied as an indicator of iron deficiency in people who have conditions that interfere with standard tests.
[175] Advanced hematology analyzers generate novel measurements of blood cells which have shown diagnostic significance in research studies but have not yet found widespread clinical use.
Analyzers that use myeloperoxidase staining to produce differential counts can measure white blood cells' expression of the enzyme, which is altered in various disorders.
[171] (4–7 years old) (0–1 days old) The complete blood count is interpreted by comparing the output to reference ranges, which represent the results found in 95% of apparently healthy people.
[179] On average, adult females have lower hemoglobin, hematocrit, and red blood cell count values than males; the difference lessens, but is still present, after menopause.
[181][183] The red blood cell count and related values begin to decline shortly after birth, reaching their lowest point at about two months of age and increasing thereafter.
If the sample is visibly clotted, which can be caused by poor phlebotomy technique, it is unsuitable for testing, because the platelet count will be falsely decreased and other results may be abnormal.
[91] Some individuals produce an antibody that causes their platelets to form clumps when their blood is drawn into tubes containing EDTA, the anticoagulant typically used to collect CBC samples.
Throughout the 18th and 19th centuries, improvements in microscope technology such as achromatic lenses allowed white blood cells and platelets to be counted in unstained samples.
[8][204][205] His technique, published in 1852, involved aspirating a carefully measured volume of blood into a capillary tube and spreading it onto a microscope slide coated with egg white.
In 1877, William Gowers invented a hemocytometer with a built-in counting grid, eliminating the need to produce specially calibrated eyepieces for each microscope.
[203] Dmitri Leonidovich Romanowsky improved on this technique in the 1890s, using a mixture of eosin and aged methylene blue to produce a wide range of hues not present when either of the stains was used alone.
[205] Attempts to automate this process using spectrophotometry and colorimetry were limited by the fact that hemoglobin is present in the blood in many different forms, meaning that it could not be measured at a single wavelength.
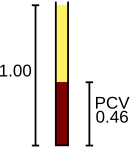
[66][212] In 1929, he undertook a PhD project at the University of Tulane to determine normal ranges for red blood cell parameters, and invented a method known as the Wintrobe hematocrit.
Hematocrit measurements had previously been described in the literature, but Wintrobe's method differed in that it used a large tube that could be mass-produced to precise specifications, with a built-in scale.
[213] Wallace's patent application was granted in 1953, and after improvements to the aperture and the introduction of a mercury manometer to provide precise control over sample size, the brothers founded Coulter Electronics Inc. in 1958 to market their instruments.
[216] They were expensive, slow, and did little to reduce workload in the laboratory because they still required blood smears to be prepared and stained, so flow cytometry-based systems became more popular,[217][218] and by 1990, no digital image analyzers were commercially available in the United States or western Europe.
This analyzer was unpopular with hematology laboratories because it was labour-intensive to operate, but in the late 1980s to early 1990s similar systems were widely produced by other manufacturers such as Sysmex, Abbott, Roche and Beckman Coulter.