Bradycardia
[1] While bradycardia can result from various pathologic processes, it is commonly a physiologic response to cardiovascular conditioning or due to asymptomatic type 1 atrioventricular block.
[5] Bradycardia may be associated with symptoms of fatigue, dyspnea, dizziness, confusion, and frank syncope due to reduced forward blood flow to the brain, lungs, and skeletal muscle.
[6] The types of symptoms often depend on the etiology of the slow heart rate, classified by the anatomic location of a dysfunction within the cardiac conduction system.
[2] Generally, these classifications involve the broad categories of sinus node dysfunction (SND), atrioventricular block, and other conduction tissue diseases.
Excess vagus nerve activity or carotid sinus hypersensitivity are neurological causes of transient symptomatic bradycardia.
[6] Untreated SND has been shown to increase the future risk of heart failure and syncope, sometimes warranting definitive treatment with an implanted pacemaker.
[citation needed] The term "relative bradycardia" can refer to a heart rate lower than expected in a particular disease state, often a febrile illness.
[8] Chronotropic incompetence (CI) refers to an inadequate rise in heart rate during periods of increased demand, often due to exercise, and is an important sign of SND and an indication for pacemaker implantation.
Like most cells, cardiomyocytes maintain a highly regulated negative voltage at rest and are capable of propagating action potentials, much like neurons.
[10] While at rest, the negative cellular voltage of a cardiomyocyte can be raised above a certain threshold (so-called depolarization) by an incoming action potential, causing the myocyte to contract.
When these contractions occur in a coordinated fashion, the atria and ventricles of the heart will pump, delivering blood to the rest of the body.
[11] The SA node contains pacemaker cells that demonstrate "automaticity" and can generate impulses that travel through the heart and create a steady heartbeat.
The His-Purkinje system conducts action potentials much faster than can be propagated between myocardial cells, allowing the entire ventricular myocardium to contract in less time, improving pump function.
[5] Cardiac action potentials are generated from the SA node and propagated through an otherwise normal conduction system, but they occur at a slow rate.
[2] Respiratory sinus arrhythmia refers to the physiologically normal variation in heart rate due to breathing.
During inspiration, vagus nerve activity decreases, reducing parasympathetic innervation of the sinoatrial node and causing an increase in heart rate.
[15] The condition can also be caused by dysfunction of the autonomic nervous system that regulates the node and is commonly exacerbated by medications.
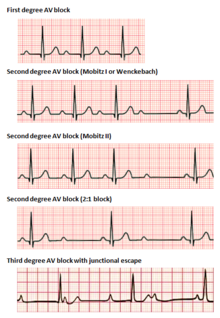
Throughout the group, the PR interval gradually lengthens until a dropped conduction occurs, resulting in no QRS complex seen on surface ECG following the last P wave.
[17] 2nd degree, Mobitz type 2 AV block is another phenomenon of intermittently dropped QRS complexes after characteristic groupings of beats seen on surface ECG.
[17] Because type 2 blocks are typically due to lesions below the AV node, the ability for ventricular escape rhythms to maintain cardiac output is compromised.
[16] An AV-junctional rhythm, or atrioventricular nodal bradycardia, is usually caused by the absence of the electrical impulse from the sinus node.
[14] Impulses originating within or below the bundle of His in the AV node will produce a wide QRS complex with heart rates between 20 and 40 BPM.
[22] At rest, although tachycardia is more commonly seen in fatty acid oxidation disorders, acute bradycardia can occur more rarely.
Ultimately, the causes act by three mechanisms: depressed automaticity of the heart, conduction block, or escape pacemakers and rhythms.
[5] Challenge with oral theophylline can be used as a diagnostic agent in people with bradycardia caused by sinus node dysfunction (SND) to help correlate symptoms.
[5] Theophylline increases resting heart rate and improves subjective symptoms in most people with bradycardia due to SND.
[5] In people who are unwilling to undergo pacemaker implantation or are not candidates for cardiac pacing, chronic oral theophylline, an adenosine receptor antagonist, can be considered for treatment of symptomatic bradycardia.
[35] However, side effects, like orthostatic hypotension with hydralazine, prazosin, and anticholinergics and myocardial toxicity with sympathomimetics, as well as limited data for this indication, hinder their routine and long-term use.
[35] If hypothyroidism is present and is the cause of symptomatic bradycardia, symptoms respond well to replacement therapy with thyroid hormone.
[34] Methylxanthines like theophylline and aminophylline are also used in the treatment of acute bradycardia due to sinus node dysfunction (SND).