Brain tumor
[2][8] Uncommon risk factors include exposure to vinyl chloride, Epstein–Barr virus, ionizing radiation, and inherited syndromes such as neurofibromatosis, tuberous sclerosis, and von Hippel-Lindau Disease.
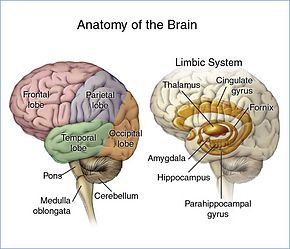
Since the frontal, temporal, and parietal lobes[14] control inhibition, emotions, mood, judgement, reasoning, and behavior, a tumor in those regions can cause inappropriate social behavior,[25] temper tantrums,[25] laughing at things which merit no laughter,[25] and even psychological symptoms such as depression and anxiety.
[8] For brain cancers that follow a CT scan at lags of 2 years or more, it has been estimated that 40% are attributable to CT-scan radiation.
[28] Inherited conditions, such as Von Hippel–Lindau disease, tuberous sclerosis, multiple endocrine neoplasia, and neurofibromatosis type 2 carry a high risk for the development of brain tumors.
[34] The claim that cell-phone usage may cause brain cancer is likely based on epidemiological studies which observed a slight increase in glioma risk among heavy users of wireless phones.
Disruption of the BBB is well imaged via MRI or CT scan, and is therefore regarded as the main diagnostic indicator for malignant gliomas, meningiomas, and brain metastases.
For example, a study was done where surgeons were able to separate benign brain tumors from malignant ones by analyzing the shapes of the blood vessels that were extracted from MRA.
[45] Although not required, some MRA may inject contrast agent, gadolinium, into the patient to get an enhanced image Magnetic Resonance Spectroscopy (MRS) – measures the metabolic changes or chemical changes inside the tumor.
The vascular morphology and degree of angiogenesis from pMRI help to determine the grade and malignancy of brain tumors.
For brain tumor diagnosis, pMRI is useful in determining the best site to perform biopsy and to help reduce sampling error.
For patients that are undergoing anti-angiogenesis cancer therapy, pMRI can give the doctors a better sense of efficacy of the treatment by monitoring tumor cerebral blood volume.
Without preoperative fMRI, the neurosurgeon would have to perform an awake-craniotomy where the patient would have to interact during open surgery to see if tumor removal would affect important brain functions.
[49] Diffusion Weighted Imaging (DWI) – a form of MRI that measures random Brownian motion of water molecules along a magnetic field gradient.
[51] Like an MRI, a contrast dye may also be injected into the veins or ingested by mouth before a CT scan to better outline any tumors that may be present.
Positron Emission Tomography (PET) Scan – uses radiolabelled substances, such as FDG which taken up by cells that are actively dividing.
It is useful after treatment to help doctors determine if the abnormal area on an MRI image is a remaining tumor or a scar tissue.
[51] Maximal safe surgical resection (to preserve as much neurological function as possible) and histologic examination of the tumor is also required to aid in the diagnosis.
[56] Tumors can be benign or malignant, can occur in different parts of the brain, and may be classified as primary or secondary.
[citation needed] Grading of the tumors of the central nervous system commonly occurs on a 4-point scale (I-IV) created by the World Health Organization in 1993.
Genetic mutations are typically detected via immunohistochemistry, a technique that visualizes the presence or absence of a targeted protein via staining.
[43] Anaplastic astrocytoma, Anaplastic oligodendroglioma, Astrocytoma, Central neurocytoma, Choroid plexus carcinoma, Choroid plexus papilloma, Choroid plexus tumor, Colloid cyst, Dysembryoplastic neuroepithelial tumour, Ependymal tumor, Fibrillary astrocytoma, Giant-cell glioblastoma, Glioblastoma, Gliomatosis cerebri, Gliosarcoma, Hemangiopericytoma, Medulloblastoma, Medulloepithelioma, Meningeal carcinomatosis, Neuroblastoma, Neurocytoma, Oligoastrocytoma, Oligodendroglioma, Optic nerve sheath meningioma, Pediatric ependymoma, Pilocytic astrocytoma, Pinealoblastoma, Pineocytoma, Pleomorphic anaplastic neuroblastoma, Pleomorphic xanthoastrocytoma, Primary central nervous system lymphoma, Sphenoid wing meningioma, Subependymal giant cell astrocytoma, Subependymoma, Trilateral retinoblastoma.
[citation needed] The goal of radiation therapy is to kill tumor cells while leaving normal brain tissue unharmed.
Hypofractionated radiation therapy has similar efficacy for survival as compared to conventional radiotherapy, particularly for individuals aged 60 and older with glioblastoma.
Dexamethasone is the preferred corticosteroid due to its long half life and reduced effect on water retention (mineralcorticoid activity).
Medulloblastoma has a good prognosis with chemotherapy, radiotherapy, and surgical resection while glioblastoma has a median survival of only 15 months even with aggressive chemoradiotherapy and surgery.
[82] Brainstem gliomas have the poorest prognosis of any form of brain cancer, with most patients dying within one year, even with therapy that typically consists of radiation to the tumor along with corticosteroids.
However, one type, focal brainstem gliomas in children, seems open to exceptional prognosis and long-term survival has frequently been reported.
Even when aggressive multimodality therapy consisting of radiotherapy, chemotherapy, and surgical excision is used, median survival is only 15–18 months.
[111][112] Led by Prof. Nori Kasahara, researchers from USC, who are now at UCLA, reported in 2001 the first successful example of applying the use of retroviral replicating vectors towards transducing cell lines derived from solid tumors.
This has been under investigation since 2010 in a Phase I/II clinical trial for the potential treatment of recurrent high-grade glioma including glioblastoma and anaplastic astrocytoma.