Oligodendroglioma
Depending on the location of the tumor, many different neurological and neuropsychological deficits can be induced, including, but not limited to, visual loss, motor weakness, cognitive decline, and anxiety.
[3] A computed tomography (CT) or magnetic resonance imaging (MRI) scan is necessary to characterize tumor size, location, and hetero- or homogeneity.
They appear as a monotonous population of mildly enlarged round cells infiltrating normal brain parenchyma and producing vague nodules.
When invading grey matter structures such as cortex, the neoplastic oligodendrocytes tend to cluster around neurons exhibiting a phenomenon referred to as "perineuronal satellitosis".
Non-classical variants and combined tumors of both oligodendroglioma and astrocytoma differentiation are seen, making this distinction controversial between different neuropathology groups.
[6] Therefore, OLIG2 should not be used to differentiate these classes of adult gliomas, although the expression level might predict the IDH mutation status in some clinical circumstances.
The ultimate responsibility for making treatment decisions and interpretation of this diagnosis lies with the oncologist in consultation with the patient and their family.
The diagnostic utility of this latter category is uncertain as these tumors may behave either like glioblastoma or grade III Anaplastic oligodendrogliomas.
The high frequency of co-deletion is a striking feature of this glial tumour and is considered as a "genetic signature" of oligodendroglioma.
Alternatively, 1p/19q loss might be an early oncogenic lesion promoting the formation of glial neoplasms, which retain high sensitivity to genotoxic stress.
Most larger cancer treatment centers routinely check for the deletion of 1p/19q as part of the pathology report for oligodendrogliomas.
In a 2019 study, an 80% survival rate was reported at 15 years for 1p/19q co-deleted oligodendroglioma treated with upfront chemotherapy irrespective of tumor grade.
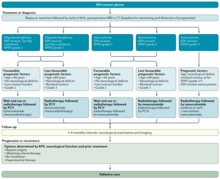
[19] Given the indolent nature of this tumor and the potential morbidity associated with neurosurgery, chemotherapy and radiation therapy, most neurooncologists will initially pursue a course of watchful waiting and treat patients symptomatically.
[19][23][24] Oligodendrogliomas, like all other infiltrating gliomas, have a very high (almost uniform) rate of recurrence and gradually increase in grade over time.
[25] With aggressive treatment and close monitoring, it is possible to outlive the typical life expectancies for low grade oligodendroglioma.
Additionally, such historic data loses significance due to the relatively long survival of patients (compared to other types of brain tumors) and the introduction of newer treatment options over time.
In a 2019 study, an 80% survival rate was reported at 15 years for 1p/19q co-deleted oligodendroglioma treated with upfront chemotherapy irrespective of tumor grade.