Cataract surgery
[2] Manual small incision cataract surgery (MSICS), which is considerably more economical in time, capital equipment, and consumables, and provides comparable results, is popular in the developing world.
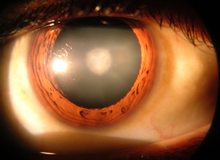
[2] Cataracts most commonly occur due to aging, but may also be caused by trauma or radiation exposure, be present since birth, or may develop as a complication of eye surgery intended to solve other health problems.
Intracapsular cataract extraction has been superseded where the facilities for surgery under a microscope are available except for cases where the lens capsule cannot be retained, and couching is no longer used in mainstream medicine.
[6] MSICS has been prioritized as the method of choice in developing countries, because it provides high-quality outcomes with less surgically-induced astigmatism than standard ECCE, no suture-related problems, quick rehabilitation, and fewer post-operative visits.
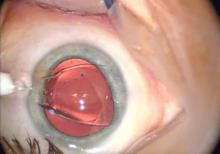
[35] Other designs of multifocal intraocular lens that focus light from distant and near objects, working with similar effect to bifocal or trifocal eyeglasses, are also available.
[42][43] Some IOLs are able to absorb ultraviolet and high-energy blue light, thus mimicking the functions of the natural crystalline lens of the eye, which usually filters potentially harmful frequencies.
General anaesthesia and retrobulbar blocks were historically used for intracapsular cataract surgery, and may be used for children and adults whose medical or psychiatric issues significantly affect their ability to remain still during the procedure.
The shape, position, and size of the incision affect the capacity for self sealing, the tendency to induce astigmatism, and the surgeon's ability to maneuvre instruments through the opening.
[52] Ophthalmic viscosurgical devices (OVDs), a class of clear, gel-like materials, are injected into the anterior chamber at the start of the procedure, to support, stabilize, and protect the eyeball, to help maintain eye shape and volume, and to distend the lens capsule during IOL implantation.
[59] The cataract's outer (cortical) layer is then separated from the capsule by a gentle, continuous flow or pulsed dose of liquid from a cannula, which is injected under the anterior capsular flap, along the edge of the capsulorhexis opening, in a step called hydrodissection.
[2] Many of the steps followed during MSICS are similar, if not identical, to those for phacoemulsification; the main differences are related to the alternative method of incision and cataract extraction from the capsule and eye.
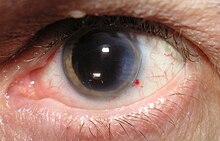
[2][73] Risk factors for posterior capsule rupture include advanced age, female sex, small capsulorhexis, small pupil opening during surgery, high myopia, pseudoexfoliation, dense cataract nucleus, posterior polar cataract, history of preoperative trauma, previous treatment for retinal disease, poor patient cooperation, and surgical inexperience.
Risk factors for suprachoroidal hemorrhage include anterior chamber intraocular lens (ACIOL), axial myopia, advanced age, atherosclerosis, glaucoma, systolic hypertension, tachycardia, uveitis and previous ocular surgery.
[80] Toxic anterior segment syndrome (TASS), a non-infectious inflammatory condition, may also occur following cataract surgery: it is usually treated with topical corticosteroids in high dosage and frequency.
It rarely occurs as a complication of cataract surgery, due to the use of prophylactic antibiotics, but there is some concern that the clear cornea incision might predispose to the increase of endophthalmitis, although no conclusive study has corroborated this suspicion.
The risk gets higher in association with factors such as diabetes, advanced age, larger incision procedures,[32] and vitreous communication with the anterior chamber caused by posterior capsule rupture.
Outcomes can be severe even with treatment, and may range from permanently decreased visual acuity to the complete loss of light perception, depending on the microbiological etiology.
[86] Mechanical pupillary block manifests when the anterior chamber gets shallower as a result of the obstruction of the aqueous humour flow through the pupil by the vitreous face or IOL.
[91] Other possible complications include elevated intraocular pressure;[87] swelling or oedema of the cornea, which is sometimes associated with transient or permanent cloudy vision (pseudophakic bullous keratopathy); displacement or dislocation of the IOL implant; unplanned high refractive error—either myopic or hypermetropic—due to errors in the ultrasonic biometry (measurement of the eye length and calculation of the required intraocular lens power); cyanopsia, which often occurs for a few days, weeks or months after removal of a cataract; and floaters, which commonly appear after surgery.
[94] Depending on the procedure, they should avoid driving for at least 24 hours after the surgery, largely due to effects from the anaesthesia, possible swelling affecting focus, and pupil dilation causing excessive glare.
[97] After full recovery, visual acuity depends on the underlying condition of the eye, the choice of IOL, and any long-term complications associated with the surgery.
[100] According to a 2009 study conducted in Sweden, factors that affected predicted refraction error included sex, pre-operative visual acuity and glaucoma, together with other eye conditions.
[104][105] Cataract surgery has a long history in Europe, Asia, and Africa, with Chrysippus of Soli, a stoic Greek philosopher providing the earliest account.
[17][15][111] In 1967, Charles Kelman introduced phacoemulsification, which uses ultrasonic energy to emulsify the nucleus of the crystalline lens and remove cataracts by aspiration without a large incision.
Remaining challenges to management of avoidable blindness include population size, gender disparities in access to eye-care, and the availability of a professional workforce.
Progress on gathering information on epidemiology, distribution and impact of cataracts within the African continent has been made, but significant problems and barriers limiting further access to reliable data remain.
[6] A 2021 study found that perioperative procedures before and after surgery differ considerably between various surgeons and institutions, which suggests the possibility for large amounts of unnecessary expenditure worldwide.
[135] As of 2015[update], the standard of care for pediatric cataract surgery for children older than two years is primary posterior intraocular lens (IOL) implantation.
[136] Research into the possibility of regeneration of infant lenses from lens epithelial cells showed interesting results in a small trial study reported in 2016.
Operating on both eyes on the same day as separate procedures is known as immediately sequential bilateral cataract surgery; this can decrease the number of hospital visits, thus reducing risk of contagion in an epidemic.