Cholecystectomy
[9] Of the more than 20 million people in the US with gallstones, only about 30% will eventually require cholecystectomy to relieve symptoms (pain) or treat complications.
[11] Typically, pain from biliary colic is felt in the right upper part of the abdomen, is moderate to severe, and goes away on its own after a few hours when the stone dislodges.
[1] Repeated attacks of biliary colic are the most common reason for removing the gallbladder, and lead to about 300,000 cholecystectomies in the US each year.
[16] Pain in cholecystitis is similar to that of biliary colic, but lasts longer than six hours and occurs together with signs of infection such as fever, chills, or an elevated white blood cell count.
While cholecystectomy is not usually the immediate treatment choice for either of these conditions, it is often recommended to prevent repeat episodes from additional gallstones getting stuck.
People can be split into high and low risk groups using a tool such as the ASA physical status classification system.
[23] In laparoscopic cholecystectomy, approximately 25–30% of biliary injuries are identified during the operation; the rest become apparent in the early post-operative period.
[28] Some reports exist of spilled stones lying unnoticed for up to 20 years before eventually causing an abscess to form.
[29] Experts agree that many biliary injuries in laparoscopic cases are caused by difficulties seeing and identifying the anatomy clearly.
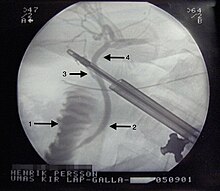
[30] Peroperative Endoscopic Retrograde Cholangio-Pancreaticography (ERCP)/ Laparo-endoscopic rendezvous (LERV) technique CBDS are found in 10–15% of patients during cholecystectomy when intraoperative cholangiography (IOC) is routinely performed.
This technique was first described in 1993 by Deslandres et al.[34] and has, in several studies, been shown to have a high rate of CBD stones clearance and a reduced number of complications, particularly post-ERCP pancreatitis, in comparison with conventional ERCP.
[35] [36] This is probably due to the facilitated access to the common bile duct with a lesser degree of manipulation and trauma to the papilla Vateri.
In a study by Swahn et al. the rendezvous method was shown to reduce the risk of PEP from 3.6 to 2.2% compared with conventional biliary cannulation.
[39] Use of prophylactic antibiotics is controversial; however, a dose may be given prior to surgery to prevent infection in certain people at high risk.
[43] Laparoscopic surgery is thought to have fewer complications, shorter hospital stay, and quicker recovery than open cholecystectomy.
For uncomplicated laparoscopic cholecystectomies, people may be discharged on the day of surgery after adequate control of pain and nausea.
If there is an inability to safely isolate the structures needed to isolate for cholecystectomy (the cystic duct and the cystic artery) for whatever reason (many times patients have part of the small bowel or colon stuck to the gallbladder, which make it dangerous to pull off without making an accidental hole in the small bowel), the surgical team may elect to do a subtotal cholecystectomy; either a fenestrated or reconstituting type.
Complications include continued output from drain, which may result in the need for ERCP stent placement to stop drainage.
In 95% of people undergoing cholecystectomy as treatment for simple biliary colic, removing the gallbladder completely resolves their symptoms.
[7] The cause is unclear, but is presumed to be due to disturbances in the biliary system that speed up enterohepatic recycling of bile salts.
The terminal ileum, the portion of the intestine where these salts are normally reabsorbed, becomes overwhelmed, does not absorb everything, and the person develops diarrhea.
[8] Early elective surgery is recommended for women with symptomatic gallstones to decrease the risk of spontaneous abortion and pre-term delivery.
[8] Without cholecystectomy, more than half of such women will have recurrent symptoms during their pregnancy, and nearly one in four will develop a complication, such as acute cholecystitis, that requires urgent surgery.
Conservative management for biliary colic involves a "watch and wait" approach—treating symptoms as-needed with oral medications.
In this procedure, an endoscope, or small, long thin tube with a camera on the end, is passed through the mouth and down the esophagus.
The doctor advances the camera through the stomach and into the first part of the small intestine to reach the opening of the bile duct.
The doctor can inject a special, radiopaque dye through the endoscope into the bile duct to see stones or other blockages on x-ray.
[59] Mühe presented his technique to the Congress of the German Surgical Society in 1986, claiming reduced postoperative pain and shorter hospitalization.
[59] Mühe's work was further disparaged in 1987, when he was charged with manslaughter for a postoperative patient death that was mistakenly attributed to his innovative technique.
[59] Driven by popularity among patients, the laparoscopic technique became preferred over open surgery and noninvasive treatments for gallstones.