Colectomy
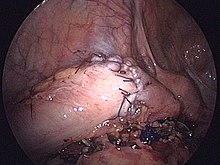
In cancer patients, lesions are commonly tattooed via colonoscopy before colectomy to give the surgeon an intraoperative visual guide.
[8] Studies have proven the feasibility of single port access colectomy, which would require only one small incision, but no clear benefit in terms of outcome or complication rate has been demonstrated.
[1] When colectomy is performed as part of damage control surgery in life-threatening trauma resulting in destructive colon injury, the surgeon may opt to leave the cut ends of the bowel sealed and disconnected for a short time to allow for further resuscitation of the patient before returning to the operating room for definitive repair (anastomosis or colostomy).
Studies have shown that differences in rates of anastomotic leak and surgical site contamination for stapled vs. sutured anastomoses are not statistically significant.
Several factors influence the risk of anastomotic dehiscence, including preservation of blood supply to the cut ends of the bowel, tension on the anastomosis, and the patient's intestinal microbiome, which affects wound healing and potential for surgical site infection.
[15] The use of NSAIDS for analgesia following gastrointestinal surgery remains controversial, given mixed evidence of an increased risk of leakage from any bowel anastomosis created.
Right-sided diverticulitis, cecal volvulus, inflammatory bowel disease, and adenomatous polyps are benign conditions that may require right hemicolectomy.
Benign indications for sigmoidectomy include diverticular disease, especially when complicated by perforation or fistulae, sigmoid volvulus, trauma, and ischemic or infectious colitis.
This is usually done out of the impossibility of performing a "double-barrel" or Mikulicz colostomy, which is preferred because it makes "takedown" (reoperation to restore intestinal continuity using an anastomosis) considerably easier.
Total colectomy is also performed for certain forms of inflammatory bowel disease, severe acute colitis, slow-transit constipation, and cancer.
Sir William Arbuthnot-Lane was one of the early proponents of the usefulness of total colectomies and was considered a pioneer of colon surgery for routinely performing this procedure.
The first reported ostomy, performed in 1776 by Pillore of Rouen as an attempt to circumvent blockage caused by a rectal tumor, was done at the insistence of the patient despite opposition from other doctors.
Dr. Robert Weir suggested in his 1886 case report on the resection of a rectal tumor that shock from the operation and leakage of intestinal contents both during and after surgery contributed to these numbers.
Primarily criticized as dangerous, Reybard's procedure went against the standard protocol of the day: resection of the colon with stoma creation and distal closure.
However, the dexterity and precision afforded by current robotic surgical technology have spurred new interest in the role of sutured anastomosis.