Diabetes
If left untreated, the disease can lead to various health complications, including disorders of the cardiovascular system, eye, kidney, and nerves.
Type 1 diabetes is an autoimmune condition where the body's immune system attacks the beta cells in the pancreas, preventing the production of insulin.
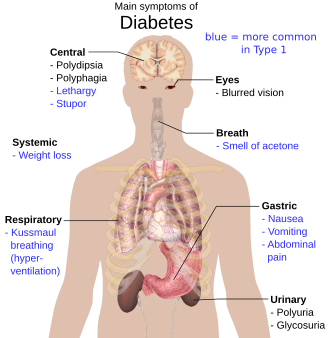
[21] Common symptoms of diabetes include increased thirst, frequent urination, extreme hunger, and unintended weight loss.
[22][23] Several other non-specific signs and symptoms may also occur, including fatigue, blurred vision, sweet smelling urine/semen and genital itchiness due to Candida infection.
[23] Loss of pain sensation predisposes to trauma that can lead to diabetic foot problems (such as ulceration), the most common cause of non-traumatic lower-limb amputation.
[33] The disease is characterized by loss of the insulin-producing beta cells of the pancreatic islets, leading to severe insulin deficiency, and can be further classified as immune-mediated or idiopathic (without known cause).
[60] The progression of prediabetes to overt type 2 diabetes can be slowed or reversed by lifestyle changes or medications that improve insulin sensitivity or reduce the liver's glucose production.
[68] Antipsychotic medication, SSRI, and SNRI side effects (specifically metabolic abnormalities, dyslipidemia and weight gain) are also potential risk factors.
Risks to the baby include macrosomia (high birth weight), congenital heart and central nervous system abnormalities, and skeletal muscle malformations.
Increased levels of insulin in a fetus's blood may inhibit fetal surfactant production and cause infant respiratory distress syndrome.
A caesarean section may be performed if there is marked fetal distress[73] or an increased risk of injury associated with macrosomia, such as shoulder dystocia.
The ICD-10 (1992) diagnostic entity, malnutrition-related diabetes mellitus (ICD-10 code E12), was deprecated by the World Health Organization (WHO) when the current taxonomy was introduced in 1999.
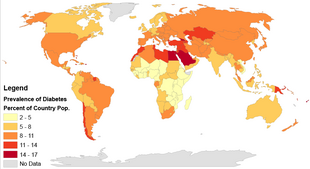
[96] Type 2 diabetes—which accounts for 85–90% of all cases worldwide—can often be prevented or delayed[97] by maintaining a normal body weight, engaging in physical activity, and eating a healthy diet.
[100] The relationship between type 2 diabetes and the main modifiable risk factors (excess weight, unhealthy diet, physical inactivity and tobacco use) is similar in all regions of the world.
There is growing evidence that the underlying determinants of diabetes are a reflection of the major forces driving social, economic and cultural change: globalization, urbanization, population aging, and the general health policy environment.
[107] Learning about the disease and actively participating in the treatment is important, since complications are far less common and less severe in people who have well-managed blood sugar levels.
[117] People with diabetes can benefit from education about the disease and treatment, dietary changes, and exercise, with the goal of keeping both short-term and long-term blood glucose levels within acceptable bounds.
[124] The studies included were mainly of very low-certainty and did not report on health-related quality of life, diabetes complications, all-cause mortality or socioeconomic effects.
During the length of a 12-month program, youth and their parents participated in 4 education sessions learning about the benefits, safe procedures, glucose control, and physical activity.
Physical activity plays a vital role in managing diabetes, improving glycemic control, and enhancing the overall quality of life for children and adolescents.
Examples of this could include anxiety about experiencing hypoglycemic events during exercise or the physical challenges posed by the long-term complications that diabetes cause.
These outcomes can include better lipid profiles (higher HDL-C and lower triglycerides), healthier body composition (reduced waist circumference and BMI), and improved overall physical health.
There is a need for targeted interventions that promote physical activity and improve CRF in youth with type 2 diabetes to help reduce the risk of long-term complications.
Future research could focus on more dire metabolic conditions like type II diabetes, investigate the role of physical maturation, and think about including longer intervention periods.
[134] Type 2 diabetes is generally treated with medication that is taken by mouth (e.g. metformin) although some eventually require injectable treatment with insulin or GLP-1 agonists.
Evidence has shown that social prescribing led to slight improvements in blood sugar control for people with type 2 diabetes.
[161] There is no adequate evidence to support effects on cholesterol, blood pressure, behavioral change (such as physical activity levels and dietary), depression, weight and health-related quality of life, nor in other biological, cognitive or emotional outcomes.
[19][39] Some data indicate rates are roughly equal in women and men,[19] but male excess in diabetes has been found in many populations with higher type 2 incidence, possibly due to sex-related differences in insulin sensitivity, consequences of obesity and regional body fat deposition, and other contributing factors such as high blood pressure, tobacco smoking, and alcohol intake.
[174] Effective treatment was not developed until the early part of the 20th century when Canadians Frederick Banting and Charles Best isolated and purified insulin in 1921 and 1922.
The principles of treatment (weight loss, oral antidiabetics, subcutaneous insulin) and management of emergencies (e.g. ketoacidosis) are similar to those in humans.