Epilepsy in children
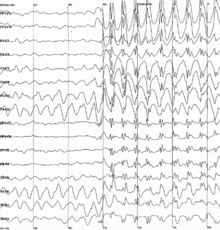
[11] As for the second criteria, an EEG test must show abnormal electrical brain patterns that indicate a high risk of recurrence of another seizure.
The consensus to set the percentage at greater than or equal to 60% is because it represents the minimum level of confidence for someone who already experienced two unprovoked seizures to likely have a third one.
[10] Multiple types of tests may be conducted in order have the most accurate diagnosis, as well as to create a personalized treatment regimen for the patient.
A high-density EEG may be used, where more electrodes are attached in order to produce a more precise, localized result of seizure activity.
[15] There is a tendency for misdiagnosing epilepsy in children, posing a challenge in establishing precise diagnosis at this life stage.
[16] Statistical parametric mapping (SPM), electrical source imaging (ESI), and magnetoencephalography (MEG) are additional analysis techniques that may be conducted to further locate the origin of the seizures.
An accurate way of classifying seizures and epilepsy types comes from obtaining a detailed patient history and performing appropriate tests and using supporting data.
[1] Factors that may contribute to a seizure episode include head injuries, recent fever or infection, concurrent health conditions, and medication.
[24] While there is limited evidence supporting their use,[26] medications used to treat infantile epilepsy have included levetiracetam, topiramate, vigabatrin, phenytoin, lamotrigine, rufinamide, stiripentol, carbamazepine, valproate, and phenobarbital.
[27] The majority of infants with epilepsy are prescribed levetiracetam and a pharmacological monotherapy treatment, with the latter representing 94% of children with onset before 34 weeks.
Medicines are selected based on the type of seizure, age of the child, side effects, cost, and ease of use.
Medications such as: stimulants, antidepressants, and antipsychotics have shown to lower seizure threshold and can increase neuro stability.
[33] In a comparative effectiveness review, levetiracetam has caused seizure freedom in some infants and is supported by a controlled trial.
In the event side effects are experienced, prescribed medications should not be stopped before discussing with the child's healthcare provider.
[1] A 2023 systematic review of the literature found limited evidence to support the effectiveness and safety of pharmacologic and dietary treatments in epilepsy in young children under three years of age.
A ketogenic diet (which features low carbohydrate/ protein consumption and high fat intake) has been suggested in infants with Dravet Syndrome and Tuberous Sclerosis and may lead to decrease seizure frequency.
[37] The ketogenic diet was a popular treatment for pediatric epilepsy prior to the discovery of anti seizure medications.
[26] It originated from the Atkins Diet which was developed to aid in weight loss but has since then been modified to further reduce carbohydrate intake and applied in treating epileptic seizures.
[40] The Low Glycemic Index Treatment (LGIT) is another form of ketogenic diet therapy that relies on skipping carbohydrates of high Glycemic Index (GI) in meals in order to avoid any abrupt rise in the blood glucose levels while allowing unconstrained consumption of fats and proteins.
Research has demonstrated that, in comparison to cKD, MAD, and MCTKD,[41] LGIT is less adverse to the cardiovascular, gastrointestinal, and genitourinary systems when used for long-term and is effective in reducing the frequency of epileptic seizures in children.
Focal resections are limited for seizure origins that are not associated with critical functions, such as vision, speech, movement, and memory.
Furthermore, this stimulation proved effective in reducing the risk of Sudden Unexpected Death in Epilepsy (SUDEP) over the long term.
A connected stimulating device is placed in the chest, underneath the skin, and works similarly to a heart pacemaker, to monitor brain activity and send electric impulses to counter seizures.
[56] The constant awareness of potential seizures can create a persistent state of alertness, leading to chronic stress.
[57] Discrimination and a lack of understanding about the condition can profoundly impact self-esteem and overall social interactions, often leading to feelings of isolation.
Open communication and education about epilepsy can foster understanding, reduce stigma, and ultimately lead to more inclusive and supportive peer relationships.
Aggression, confusion, and hyperactivity in children with epilepsy are signs of pre-ictal psychiatric symptoms that are considered to be associated with limbic system disturbances, particularly in the amygdala.
Based on the aforementioned, it is imperative that healthcare providers take into account the psychological state of children with epilepsy by meticulously selecting the best medication option that has a lower impact on their mental health and a higher treating efficacy, as well as by offering extra support to improve their mental well-being.
Currently, ECS mapping is the standard of care in localization of areas involved in focal seizure onset and pre surgical planning.
"[63] The effects of epilepsy on language may be impacted by location of epileptiform activity, severity and duration of electrical discharges, age of onset, treatment method, and surgical resection areas.