Quinolone antibiotic
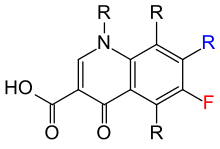
Quinolone antibiotics constitute a large group of broad-spectrum bacteriocidals that share a bicyclic core structure related to the substance 4-quinolone.
[2] Nearly all quinolone antibiotics in use are fluoroquinolones, which contain a fluorine atom in their chemical structure and are effective against both Gram-negative and Gram-positive bacteria.
However, for serious acute cases of pyelonephritis or bacterial prostatitis where the person may need to be hospitalised, fluoroquinolones are recommended as first-line therapy.
Their antibiofilm activity is generally higher than that of old beta-lactams and glycopeptides but remains lower compared to antibiotics such as tetracyclines, daptomycin, and fosfomycin, which demonstrate greater efficacy against biofilms.
[8] In most countries, fluoroquinolones are approved for use in children only under narrowly defined circumstances, owing in part to the observation of high rates of musculoskeletal adverse events in fluoroquinolone-treated juvenile animals.
[10][11][12] Fluoroquinolone use in children may be appropriate when the infection is caused by multidrug-resistant bacteria, or when alternative treatment options require parenteral administration and oral therapy is preferred.
[15][16] In a “Report to Prevent Future Deaths,” mandated by UK law, one of the coroners noted that there is no compelling reason why patients should expect to risk becoming suicidal from an antibiotic unless this fact and potential symptoms were brought to their attention by the prescriber.
[15] A 2024 review from the UK’s Medicines & Healthcare Products Regulatory Agency examined the effectiveness of current measures to reduce these identified risks of fluoroquinolones.
It concluded, “Systemic fluoroquinolones must now only be prescribed when other commonly recommended antibiotics are inappropriate.” [17] Nervous-system effects include insomnia, restlessness, and rarely, seizure,convulsions, and psychosis.
[23] In 2016, the FDA found that systemic use (by mouth or injection) of fluoroquinolones was associated with "disabling and potentially permanent serious side effects" involving the tendons, muscles, joints, nerves, and central nervous system, concluding that these side effects generally outweigh the benefits for people with acute sinusitis, acute bronchitis, and uncomplicated urinary tract infections when other treatment options are available.
[26] Clostridioides difficile colitis may occur in connection with the use of any antibacterial drug, especially those with a broad spectrum of activity such as clindamycin, cephalosporins, and fluoroquinolones.
Postmarketing surveillance has revealed a variety of relatively rare but serious adverse effects associated with all members of the fluoroquinolone antibacterial class.
Among these, tendon problems and exacerbation of the symptoms of the neurological disorder myasthenia gravis are the subject of "black box" warnings in the United States.
[44] In 2019 study by Journal of the American College of Cardiology it was discovered that fluoroquinolones could increase the risk for heart valve diseases.
[50] Other drugs that interact with fluoroquinolones include sucralfate, probenecid, cimetidine, theophylline, warfarin, antiviral agents, phenytoin, cyclosporine, rifampin, pyrazinamide, and cycloserine.
[51] Fluoroquinolones have varying specificity for cytochrome P450, so may have interactions with drugs cleared by those enzymes; the order from most P450-inhibitory to least, is enoxacin > ciprofloxacin > norfloxacin > ofloxacin, levofloxacin, trovafloxacin, gatifloxacin, moxifloxacin.
[70] In gram-negative bacteria, plasmid-mediated resistance genes produce proteins that can bind to DNA gyrase, protecting it from the action of quinolones.
With the ligase activity disrupted, these enzymes release DNA with single- and double-strand breaks that lead to cell death.
[72] The majority of quinolones in clinical use are fluoroquinolones, which have a fluorine atom attached to the central ring system, typically at the 6-position or C-8 position.
[75] Fluoroquinolones can enter in cells easily via porins, so are often used to treat intracellular pathogens such as Legionella pneumophila and Mycoplasma pneumoniae.
[83] Nalidixic acid is thus considered to be the predecessor of all members of the quinolone family, including the second, third and fourth generations commonly known as fluoroquinolones.
[85] Reports of serious adverse events began emerging, and the FDA first added a black-box warning to fluoroquinolones in July 2008 for the increased risk of tendinitis and tendon rupture.
In August 2013, the agency required updates to the labels to describe the potential for irreversible peripheral neuropathy (serious nerve damage).
The advisory committee concluded that the serious risks associated with the use of fluoroquinolones for these types of uncomplicated infections generally outweighed the benefits for patients with other treatment options.
[85][86][87][88][89] The 21-member joint committee overwhelmingly recommended stronger label warnings on the containers because of rare but sometimes devastating side effects.
[90] On 12 May 2016, the FDA issued a drug safety communication advising that fluoroquinolones should be reserved for these conditions only when no other options are available due to potentially permanent, disabling side effects occurring together.
[85] The first generation of the quinolones began following introduction of the related, but structurally distinct naphthyridine-family nalidixic acid in 1962 for treatment of UTIs in humans.
[91] Nalidixic acid was discovered by George Lesher and coworkers in a chemical distillate during an attempt at synthesis of the chloroquinoline antimalarial agent, chloroquine.
The majority of quinolones in clinical use belong to the second generation class of "fluoroquinolones", which have a true quinoline framework, maintain the C-3 carboxylic acid group, and add a fluorine atom to the all-carbon containing ring, typically at the C-6 or C-8 positions.