Glomerular filtration rate
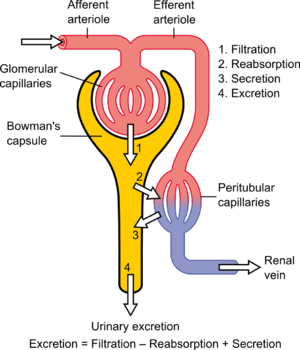
[4] Central to the physiologic maintenance of GFR is the differential basal tone of the afferent (input) and efferent (output) arterioles (see diagram).
[citation needed] GFR is equal to the renal clearance rate when any solute is freely filtered and is neither reabsorbed nor secreted by the kidneys.
It is freely filtered by the glomerulus, but also actively secreted by the peritubular capillaries in very small amounts such that creatinine clearance overestimates actual GFR by 10–20%.
All of the estimating equations depend on a prediction of the 24-hour creatinine excretion rate, which is a function of muscle mass which is quite variable.
[5] Using inulin to measure kidney function is the "gold standard" for comparison with other means of estimating glomerular filtration rate.
[6] In 2018, the French pharmacovigilance agency withdrew inulin and sinistrin-based products from the market after some patients experienced hypersensitivity reactions including a fatal outcome.
These come close to the ideal properties of inulin (undergoing only glomerular filtration) but can be measured more practically with only a few urine or blood samples.
[13] Problems with creatinine (varying muscle mass, recent meat ingestion (much less dependent on the diet than urea), etc.)
After filtration, Cystatin C is reabsorbed and catabolized by the tubular epithelial cells, with only small amounts excreted in the urine.
It is freely filtered by the glomerulus, but also actively secreted by the peritubular capillaries in very small amounts such that creatinine clearance overestimates actual GFR by 10–20%.
All of the estimating equations depend on a prediction of the 24-hour creatinine excretion rate, which is a function of muscle mass which is quite variable.
"[20] A number of formulae have been devised to estimate GFR or Ccr values on the basis of serum creatinine levels.
[22][23] The formula, as originally published, is: When serum creatinine is measured in μmol/L: One interesting feature of the Cockcroft and Gault equation is that it shows how dependent the estimation of CCr is based on age.
Another formula for calculating the GFR is the one developed by the Modification of Diet in Renal Disease Study Group.
[24] Most laboratories in Australia,[25] and the United Kingdom now calculate and report the estimated GFR along with creatinine measurements and this forms the basis of diagnosis of chronic kidney disease.
[28][29][30] The most commonly used formula is the "4-variable MDRD", which estimates GFR using four variables: serum creatinine, age, ethnicity, and gender.
When looking at NHANES (National Health and Nutrition Examination Survey) data, the median estimated GFR was 94.5 mL/min per 1.73 m2 vs. 85.0 mL/min per 1.73 m2, and the prevalence of chronic kidney disease was 11.5% versus 13.1%.
As separate equations for different populations: For creatinine (IDMS calibrated) in mg/dL: Another estimation tool to calculate GFR is the Mayo Quadratic formula.
This formula was developed by Rule et al.,[32] in an attempt to better estimate GFR in patients with preserved kidney function.
The NKDEP program in the United States has attempted to solve this problem by trying to get all laboratories to calibrate their measures of creatinine to a "gold standard", which in this case is isotope dilution mass spectrometry (IDMS).
[citation needed] The normal range of GFR, adjusted for body surface area, is 100–130 average 125 mL/min/1.73m2 in men and 90–120 ml/min/1.73m2 in women younger than the age of 40.
The most important items in a physical examination are signs of vasculitis, lupus erythematosus, diabetes, endocarditis and hypertension.
Renal enlargement usually indicates diabetic nephropathy, focal segmental glomerular sclerosis or myeloma.
[citation needed] Risk factors for kidney disease include diabetes, high blood pressure, family history, older age, ethnic group and smoking.
But significant decline of the GFR from a previous test result can be an early indicator of kidney disease requiring medical intervention.
The sooner kidney dysfunction is diagnosed and treated the greater odds of preserving remaining nephrons, and preventing the need for dialysis.
Not all clinicians agree with the above classification, suggesting that it may mislabel patients with mildly reduced kidney function, especially the elderly, as having a disease.
Hoenig et al said on the topic "Race is a social construct that cannot be measured, can be used imprecisely and may contribute to disparities in kidney transplant access for Black patients.
Explanations that have been given for this finding include the notion that black people release more creatinine into their blood at baseline, in part because they are reportedly more muscular.
They concluded saying "As long as uncertainty persists about the cause of racial differences in serum creatinine levels, we should favor practices that may alleviate health inequities over those that may exacerbate them.