Cardiac arrest
Additional factors that may contribute to cardiac arrest include major blood loss, lack of oxygen, electrolyte disturbance (such as very low potassium), electrical injury, and intense physical exercise.
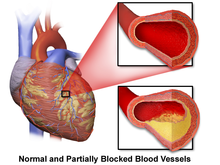
[25][26][27][28] Current cigarette smokers with coronary artery disease were found to have a two to threefold increase in the risk of sudden death between ages 30 and 59.
[35] Indeed, postmortem examinations have shown that the most common finding in cases of sudden cardiac death is chronic, high-grade stenosis of at least one segment of a major coronary artery.
[39][30] This is most commonly the result of longstanding high blood pressure, or hypertension, which has led to maladaptive overgrowth of muscular tissue of the left ventricle, the heart's main pumping chamber.
[30] The genetic mutations often affect specialized proteins known as ion channels that conduct electrically charged particles across the cell membrane, and this group of conditions is therefore often referred to as channelopathies.
[29] Additionally, individuals with LQTS should avoid certain medications that carry the risk of increasing the severity of this conduction abnormality, such as certain anti-arrhythmics, anti-depressants, and quinolone or macrolide antibiotics.
[3][48][49] Additional non-cardiac causes include hemorrhage, aortic rupture, hypovolemic shock, pulmonary embolism, poisoning such as from the stings of certain jellyfish, and electrical injury.
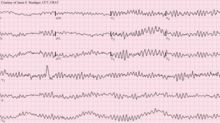
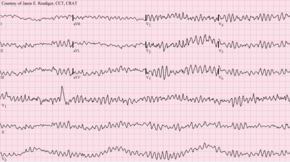
The definitive electrical mechanisms of cardiac arrest, which may arise from any of the functional, structural, or physiologic abnormalities mentioned above, are characterized by arrhythmias.
These are rapid and erratic arrhythmias that alter the circulatory pathway such that adequate blood flow cannot be sustained and is inadequate to meet the body's needs.
[59] However, structural changes in the diseased heart as a result of inherited factors (mutations in ion-channel coding genes, for example) cannot explain the sudden onset of cardiac arrest.
[30] The provider taking the person's clinical history should try to learn whether the episode was observed by anyone else, when it happened, what the patient was doing (in particular whether there was any trauma), and whether drugs were involved.
EKG readings will help to identify the arrhythmia present and allow the team to monitor any changes that occur with the administration of CPR and defibrillation.
[65] Moreover, in the post-resuscitation patient, a 12-lead EKG can help identify some causes of cardiac arrest, such as STEMI which may require specific treatments.
[68] Owing to the inaccuracy diagnosis solely based on central pulse detection, some bodies like the European Resuscitation Council have de-emphasized its importance.
[17] They have suggested that the technique to check carotid pulses should be used only by healthcare professionals with specific training and expertise, and even then that it should be viewed in conjunction with other indicators like agonal respiration.
The approach to primary prevention promotes a healthy diet, exercise, limited alcohol consumption, and smoking cessation.
[72] The study found that those who fell under the category of having "Southern [United States] diets" representing those of "added fats, fried food, eggs, organ and processed meats, and sugar-sweetened beverages" had a positive association with an increased risk of cardiac arrest, while those deemed following the "Mediterranean diets" had an inverse relationship regarding the risk of cardiac arrest.
[73] A Cochrane review published in 2016 found moderate-quality evidence to show that blood pressure-lowering drugs do not reduce the risk of sudden cardiac death.
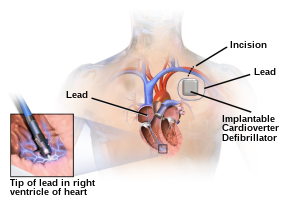
[77] Prevention of SCD with ICD therapy for high-risk patient populations has similarly shown improved survival rates in several large studies.
The high-risk patient populations in these studies were defined as those with severe ischemic cardiomyopathy (determined by a reduced left ventricular ejection fraction (LVEF)).
[91] Tracheal intubation has not been found to improve survival rates or neurological outcomes in cardiac arrest,[84][92] and in the prehospital environment, may worsen it.
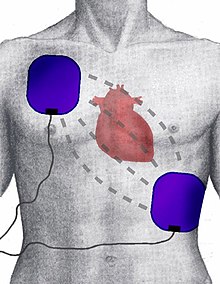
A defibrillator — either implanted or external — delivers an electrical current that results in the entire myocardium simultaneously depolarized thereby stopping the arrhythmia.
Some defibrillators even provide feedback on the quality of CPR compressions, encouraging the lay rescuer to press the person's chest hard enough to circulate blood.
Overall, calcium is not routinely used during cardiac arrest as it does not provide additional benefit (compared to non-use) and may even cause harm (poor neurologic outcomes).
However, the 2010 guidelines from the American Heart Association removed the recommendation for atropine use in pulseless electrical activity and asystole for lack of evidence supporting its use.
[119] Tricyclic antidepressant (TCA) overdose can lead to cardiac arrest with typical ECG findings including wide QRS and prolonged QTc.
[88] Current international guidelines suggest cooling adults after cardiac arrest using targeted temperature management (TTM) with the goal of improving neurological outcomes.
These protocols are often initiated by a code blue, which usually denotes impending or acute onset of cardiac arrest or respiratory failure.
[82] The precordial thump may be considered in those with witnessed, monitored, unstable ventricular tachycardia (including pulseless VT) if a defibrillator is not immediately ready for use, but it should not delay CPR and shock delivery or be used in those with unwitnessed OHCA.
[30] Additional causes of sudden unexplained cardiac arrest in children include hypertrophic cardiomyopathy and coronary artery abnormalities.