Hepatorenal syndrome
Hepatorenal syndrome (HRS) is a life-threatening medical condition that consists of rapid deterioration in kidney function in individuals with cirrhosis or fulminant liver failure.
The risk of death in hepatorenal syndrome is very high; the mortality of individuals with type 1 HRS is over 50% over the short term, as determined by historical case series.
Type 2 HRS is thought to be part of a spectrum of illness associated with increased pressures in the portal vein circulation, which begins with the development of fluid in the abdomen (ascites).
As these phenomena may not necessarily produce symptoms until late in their course, individuals with hepatorenal syndrome are typically diagnosed with the condition on the basis of altered laboratory tests.
Most people who develop HRS have cirrhosis, and may have signs and symptoms of the same, which can include jaundice, altered mental status, evidence of decreased nutrition, and the presence of ascites.
Consequently, it is a challenge to distinguish hepatorenal syndrome from other entities that cause kidney failure in the setting of advanced liver disease.
In contrast to HRS, however, pre-renal kidney failure usually responds to treatment with intravenous fluids, resulting in reduction in serum creatinine and increased excretion of sodium.
[3] Acute tubular necrosis (ATN) involves damage to the tubules of the kidney, and can be a complication in individuals with cirrhosis, because of exposure to toxic medications or the development of decreased blood pressure.
[15] Many vasoactive chemicals have been hypothesized as being involved in mediating the systemic hemodynamic changes, including atrial natriuretic factor,[16] prostacyclin, thromboxane A2,[17] and endotoxin.
[4][5] Also, large volume paracentesis—which is the removal of ascites fluid from the abdomen using a needle or catheter in order to relieve discomfort—may cause enough alteration in hemodynamics to precipitate HRS, and should be avoided in individuals at risk.
[24] Individuals with HRS and evidence of greater hepatic dysfunction (quantified as MELD scores above 36) have been found to be at greatest risk of early mortality after liver transplantation.
[1][2] In anticipation of liver transplantation (which may be associated with considerable in-hospital delay), several other strategies have been found to be beneficial in preserving kidney function.
[2] Many major studies showing improvement in kidney function in patients with hepatorenal syndrome have involved expansion of the volume of the plasma with albumin given intravenously.
[2][28] Midodrine is an alpha-agonist and octreotide is an analogue of somatostatin, a hormone involved in regulation of blood vessel tone in the gastrointestinal tract.
[30] Another nonrandomized, observational study of individuals with HRS treated with subcutaneous octreotide and oral midodrine showed that there was increased survival at 30 days.
[1][31] The vasopressin analogue ornipressin was found in a number of studies to be useful in improvement of kidney function in patients with hepatorenal syndrome,[1][25][32] but has been limited in its use, as it can cause severe ischemia to major organs.
[1][25] Terlipressin is a vasopressin analogue that has been found in one large study to be useful for improving kidney function in patients with hepatorenal syndrome with a lesser incidence of ischemia.
[1][26] A randomized control trial led by Florence Wong demonstrated improved renal function in individuals with Type 1 HRS treated with terlipressin and albumin over placebo.
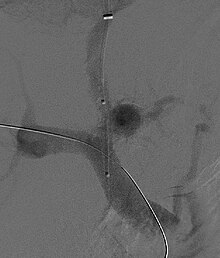
Theoretically, a decrease in portal pressures is thought to reverse the hemodynamic phenomena that ultimately lead to the development of hepatorenal syndrome.
[8][38][39] Complications of TIPS for treatment of HRS include the worsening of hepatic encephalopathy (as the procedure involves the forced creation of a porto-systemic shunt, effectively bypassing the ability of the liver to clear toxins), inability to achieve adequate reduction in portal pressure, and bleeding.
The molecular adsorbents recirculation system (MARS) has shown some utility as a bridge to transplantation in patients with hepatorenal syndrome, yet the technique is still nascent.
[8][40] Renal replacement therapy may be required to bridge individuals with hepatorenal syndrome to liver transplantation, although the condition of the patient may dictate the modality used.
[9] Three independent risk factors for the development of HRS in cirrhotics have been identified: liver size, plasma renin activity, and serum sodium concentration.
[1][43] The syndrome was soon re-associated with advanced liver disease,[23] and, in the 1950s, was clinically defined by Sherlock, Hecker, Papper, and Vessin as being associated with systemic hemodynamic abnormalities and high mortality.
The more recent history of HRS has involved elucidation of the various vasoactive mediators that cause the splanchnic and kidney blood flow abnormalities of the condition.