Hypercholesterolemia
[1] Elevated levels of non-HDL cholesterol and LDL in the blood may be a consequence of diet, obesity, inherited (genetic) diseases (such as LDL receptor mutations in familial hypercholesterolemia), or the presence of other diseases such as type 2 diabetes and an underactive thyroid.
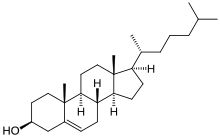
Since cholesterol is insoluble in water, it is transported in the blood plasma within protein particles (lipoproteins).
[6][7] In people with very high cholesterol (e.g., familial hypercholesterolemia), diet is often not sufficient to achieve the desired lowering of LDL, and lipid-lowering medications are usually required.
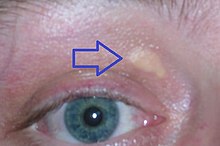
For example, familial hypercholesterolemia (Type IIa hyperlipoproteinemia) may be associated with xanthelasma palpebrarum (yellowish patches underneath the skin around the eyelids),[13] arcus senilis (white or gray discoloration of the peripheral cornea),[14] and xanthomata (deposition of yellowish cholesterol-rich material) of the tendons, especially of the fingers.
[19][20] A diet high in sugar or saturated fats increases total cholesterol and LDL.
For people at high risk of cardiovascular disease, the recommended limit for total cholesterol is 4 mmol/L, and 2 mmol/L for LDL.
[34] There is no absolute cutoff between normal and abnormal cholesterol levels, and values must be considered in relation to other health conditions and risk factors.
[38] Levels of LDL or non-HDL cholesterol both predict future coronary heart disease; which is the better predictor is disputed.
Newer methods, such as "lipoprotein subclass analysis", have offered significant improvements in understanding the connection between atherosclerosis progression and clinical consequences.
[44] The U.S. Preventive Services Task Force in 2008 strongly recommended routine screening for men 35 years and older and women 45 years and older for lipid disorders and the treatment of abnormal lipids in people at increased risk of coronary heart disease.
[10] Lifestyle changes recommended for those with high cholesterol include: smoking cessation, limiting alcohol consumption, increasing physical activity, and maintaining a healthy weight.
[8] Eating a diet with a high proportion of vegetables, fruit, dietary fiber, and low in fats results in a modest decrease in total cholesterol.
[57] However, in 2015 the Dietary Guidelines Advisory Committee in the United States removed its recommendation of limiting cholesterol intake.
[63][7] Trans fats are recognized as a potential risk factor for cholesterol-related cardiovascular disease, and avoiding them in an adult diet is recommended.
[8] Changes in total fat intake in low-calorie diets do not appear to affect blood cholesterol.
[75] Statins may improve quality of life when used in people without existing cardiovascular disease (i.e. for primary prevention).
[74] Statins decrease cholesterol in children with hypercholesterolemia, but no studies as of 2010 show improved outcomes[76] and diet is the mainstay of therapy in childhood.
[78] In the US, guidelines exist from the National Cholesterol Education Program (2004)[79] and a joint body of professional societies led by the American Heart Association.
[80] In the UK, the National Institute for Health and Clinical Excellence has made recommendations for the treatment of elevated cholesterol levels, published in 2008,[77] and a new guideline appeared in 2014 that covers the prevention of cardiovascular disease in general.
[39] Among people whose life expectancy is relatively short, hypercholesterolemia is not a risk factor for death by any cause including coronary heart disease.
[82] The American College of Physicians recommends the following for hypercholesterolemia in people with diabetes:[83] A 2002 survey found that 1.1% of U.S. adults who used alternative medicine did so to treat high cholesterol.
Some researchers, however, are concerned about diet supplementation with plant sterol esters and draw attention to the lack of long-term safety data.
[10] Rates of coronary artery disease are high in Great Britain, but low in rural China and Japan.