Hormone replacement therapy
[1] Although both classes of hormones can have symptomatic benefit, progestogen is specifically added to estrogen regimens, unless the uterus has been removed, to avoid the increased risk of endometrial cancer.
"[9] These are mainly manufactured from plant steroids[10] and can be a component of either registered pharmaceutical or custom-made compounded preparations, with the latter generally not recommended by regulatory bodies due to their lack of standardization and formal oversight.
[12] The current indications for use from the United States Food and Drug Administration (FDA) include short-term treatment of menopausal symptoms, such as vasomotor hot flashes or vaginal atrophy, and prevention of osteoporosis.
[13] Approved uses of HRT in the United States include short-term treatment of menopausal symptoms such as hot flashes and vaginal atrophy, and prevention of osteoporosis.
Menopause is the permanent cessation of menstruation resulting from loss of ovarian follicular activity, defined as beginning twelve months after the final natural menstrual cycle.
[25] This adds to a growing body of research highlighting hormone therapy’s effectiveness, not only for heart health but also for managing menopausal symptoms like hot flashes, disrupted sleep, vaginal dryness, and painful intercourse.
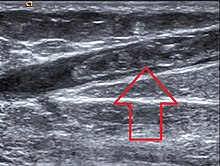
[21] Estrogen replacement can restore vaginal cells, pH levels, and blood flow to the vagina, all of which tend to deteriorate at the onset of menopause.
[6] A Cochrane review suggested that women starting HRT less than 10 years after menopause had lower mortality and coronary heart disease, without any strong effect on the risk of stroke and pulmonary embolism.
Beyond this, HRT improves heart contraction, coronary blood flow, sugar metabolism, and decreases platelet aggregation and plaque formation.
Low sex hormone-binding globulin, which occurs with menopause, is associated with increased body mass index and risk for type 2 diabetes.
[8] Ischemic stroke risk was increased during the time of intervention in the WHI, with no significant effect after the cessation of therapy[31] and no difference in mortality at long term follow up.
[6] When oral synthetic estrogen or combined estrogen-progestogen treatment is delayed until five years from menopause, cohort studies in Swedish women have suggested an association with hemorrhagic and ischemic stroke.
[6] The risk may be reduced with bioidentical progesterone,[61] though the only prospective study that suggested this was underpowered due to the rarity of breast cancer in the control population.
[67] It has been suggested by some that the absence of significant effect in some of these studies could be due to selective prescription to overweight women who have higher baseline estrone, or to the very low progesterone serum levels after oral administration leading to a high tumor inactivation rate.
[79] There appears to be a significantly decreased risk of cervical squamous cell cancer in post menopausal women treated with HRT and a weak increase in adenocarcinoma.
[86] With regards to treatment, randomized trials have shown that HRT improves executive and attention processes outside of the context of dementia in postmenopausal women, both in those that are asymptomatic and those with mild cognitive impairment.
[90] Clinical trials have also shown testosterone replacement to be associated with small statistically significant improvements in verbal learning and memory in postmenopausal women.
[92][93] The following are absolute and relative contraindications to HRT:[94] The extraction of CEEs from the urine of pregnant mares led to the marketing in 1942 of Premarin, one of the earlier forms of estrogen to be introduced.
This WHI estrogen-plus-progestin trial was stopped prematurely in 2002 because preliminary results suggested risks of combined CEEs and progestins exceeded their benefits.
The authors of the study recommended that women with non-surgical menopause take the lowest feasible dose of hormones for the shortest time to minimize risk.
The results were almost universally reported as risks and problems associated with HRT in general, rather than with Prempro, the specific proprietary combination of CEEs and MPA studied.
While there was a 23% decreased incidence of breast cancer in the estrogen-only study participants, risks of stroke and pulmonary embolism were increased slightly, predominantly in patients who began HRT over the age of 60.
This in turn prevents an increase in clotting factors and accumulation of anti-estrogenic metabolites, resulting in fewer adverse side effects, particularly with regard to cardiovascular disease and stroke.
[132] Some practitioners recommending compounded bioidentical HRT also use salivary or serum hormonal testing to monitor response to therapy, a practice not endorsed by current clinical guidelines in the United States and Europe.
[133] Bioidentical hormones in pharmaceuticals may have very limited clinical data, with no randomized controlled prospective trials to date comparing them to their animal derived counterparts.
National Institute for Health and Care Excellence guideline 1.4.8 states: "consider testosterone supplementation for menopausal women with low sexual desire if HRT alone is not effective".
[136][137][138] The documents showed that Wyeth commissioned dozens of ghostwritten reviews and commentaries that were published in medical journals to promote unproven benefits of its HRT products, downplay their harms and risks, and cast competing therapies in a negative light.
[138] The publications defended unsupported cardiovascular "benefits" of its products, downplayed risks such as breast cancer, and promoted off-label and unproven uses like prevention of dementia, Parkinson's disease, vision problems, and wrinkles.
[137] In addition, Wyeth emphasized negative messages against the SERM raloxifene for osteoporosis, instructed writers to stress the fact that "alternative therapies have increased in usage since the WHI even though there is little evidence that they are effective or safe...", called into question the quality and therapeutic equivalence of approved generic CEE products, and made efforts to spread the notion that the unique risks of CEEs and MPA were a class effect of all forms of menopausal HRT: "Overall, these data indicate that the benefit/risk analysis that was reported in the Women's Health Initiative can be generalized to all postmenopausal hormone replacement therapy products.
[142] The positive perceptions of many physicians of HRT in spite of large trials showing risks that potentially outweigh any benefits may be due to the efforts of pharmaceutical companies like Wyeth, according to May and May (2012) and Fugh-Berman (2015).