Inguinal hernia surgery
Inguinal hernia, which results from lower abdominal wall weakness or defect,[2] is more common among men with about 90% of total cases.
[1] Inguinal hernia can make a small lump in the groin region which can be detected during a physical exam and verified by imaging techniques such as computed tomography (CT).
[5] In occult (hidden) hernia, the bulge cannot be detected by physical examination and magnetic resonance imaging (MRI) can be more helpful in this situation.
Incarceration occurs when intra-abdominal fat or small intestine becomes stuck within the canal and cannot slide back into the abdominal cavity either on its own or with manual maneuvers.
Left untreated, incarceration may progress to bowel strangulation as a result of restricted blood supply to the trapped segment of small intestine causing that portion to die.
[11] Successful outcomes of repair are usually measured via rates of hernia recurrence, pain and subsequent quality of life.
[19][20] Surgery is offered to the majority of people who: Symptomatic hernias tend to cause pain or discomfort within the groin region that may increase with exertion and improve with rest.
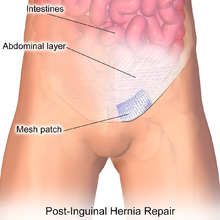
Examples of such include:[19][10][12] Techniques to repair inguinal hernias fall into two broad categories termed "open" and "laparoscopic".
Surgeons tailor their approach by taking into account factors such as their own experience with either techniques, the features of the hernia itself, and the person's anesthetic needs.
[citation needed] The IES asserts that hospital and societal costs are lower for laparoscopic repairs as compared to open approaches.
They recommend the routine use of reusable instruments as well as improving the proficiency of surgeons to help further decrease costs as well as time spent in the OR.
Repairs not using prosthetic mesh are preferable options in patients with an above-average risk of infection such as cases where the bowel has become strangulated (blood supply lost due to constriction).
Meshes made of mosquito net cloth, in copolymer of polyethylene and polypropylene have been used for low-income patients in rural India and Ghana.
The European Hernia Society recommends that in cases where an open approach is indicated, the Lichtenstein technique be utilized as the preferred method.
[44][45][46] The plug and patch tension-free technique has fallen out of favor due to higher rates of mesh shift along with its tendency to irritate surrounding tissue.
Despite being the superior non-mesh technique, the Shouldice method results much higher rates of hernia recurrence in patients when compared to repairs that utilize mesh.
[49][50] In this technique, the conjoint tendon (formed by the distal ends of the transversus abdominis and internal oblique muscles) is approximated to the inguinal ligament and closed.
All that said, many surgeons are shifting to using laparoscopic techniques as they require smaller incisions, and result in less bleeding, lower infection rates, faster recovery, shorter hospitalization periods, and reduced chronic pain.
[70][71] Studies have demonstrated that men whose hernias cause little to no symptoms can safely continue to delay surgery until a time that is most convenient for patients and their healthcare team.
[81][20][9][21] Watchful waiting requires that patients maintain a close follow-up schedule with providers to monitor the course of their hernia for any changes in symptoms and can be safely offered for up to 2 years.
[82][11] Patients who do elect watchful waiting eventually undergo repair within five years as 25% will experience a progression of symptoms such as worsening of pain.
Elective repair discussions should be revisited if patients begin to avoid aspects of their normal routine due to their hernia.
[citation needed] Inguinal hernia repair complications are unusual, and the procedure as a whole proves to be relatively safe for the majority of patients.
Risks inherent in almost all surgical procedures include:[9] Risks that are specific to inguinal hernia repairs include such things as:[9][17][21] Post-herniorrhaphy inguinodynia is a condition where 10-12% of patients experience severe pain after inguinal hernia repair, due to a complex combination of different forms of pain signals.
[12] Most patients can resume their normal routine of daily living within the week such as driving, showering, light lifting, as well as sexual activity.
[99] Post-op development of any of the following should warrant timely reporting via phone:[25][17] Most indirect inguinal hernias in the abdominal wall are not preventable.