Corneal transplantation
The graft is taken from a recently deceased individual with no known diseases or other factors that may affect the chance of survival of the donated tissue or the health of the recipient.
[1][2] Corneal transplantation is performed when medicines, keratoconus conservative surgery and cross-linking can no longer heal the cornea.
Since the cornea has no blood vessels (it takes its nutrients from the aqueous humor) it heals much more slowly than a cut on the skin.
[11] Prior to the development of reliable HIV testing, many countries instituted bans on corneal donation by gay men.
The doctor might also perform a physical examination and order lab tests, such as blood work, X-rays, or an EKG.
Antibiotic eyedrops are placed, the eye is patched, and the patient is taken to a recovery area while the effects of the anesthesia wear off.
Disadvantages include the technically challenging nature of these procedures, which replace portions of a structure only 500 μm thick, and reduced optical performance of the donor/recipient interface compared to full-thickness keratoplasty.
Patients may recover functional vision in days to weeks, as opposed to up to a year with full thickness transplants.
However, an Australian study has shown that despite its benefits, the loss of endothelial cells that maintain transparency is much higher in DSEK compared to a full-thickness corneal transplant.
In the immediate postoperative period the donor tissue is held in position with an air bubble placed inside the eye (the anterior chamber).
Gradual reduction in endothelial cell density over time can lead to loss of clarity and require repeating the procedure.
The main advantages of synthetic corneas are that they are biocompatible, and the network between the parts and the device prevents complications that could arise at their interface.
[17] In a very rare and complex multi-step surgical procedure, employed to help the most disabled patients, a lamina of the person's tooth is grafted into the eye, with an artificial lens installed in the transplanted piece.
[clarification needed] The prognosis for visual restoration and maintenance of ocular health with corneal transplants is generally very good.
The majority of corneal transplants result in significant improvement in visual function for many years or a lifetime.
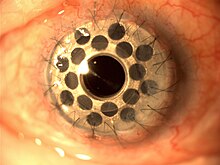
In this procedure, an ophthalmologist makes an incision in the cornea of the eye, and inserts two crescent or semi-circular shaped ring segments between the layers of the corneal stroma, one on each side of the pupil.
[18] Intrastromal corneal rings were approved in 2004 by the Food and Drug Administration for people with keratoconus who cannot adequately correct their vision with glasses or contact lenses.
[22] Although approximately 100,000 procedures are performed worldwide each year, some estimates report that 10,000,000 people are affected by various disorders that would benefit from corneal transplantation.
Russian eye surgeon Vladimir Filatov's attempts at transplanting cornea started with the first try in 1912 and were continued, gradually improving until on 6 May 1931 he successfully grafted a patient using corneal tissue from a deceased person.
[28][29] Tudor Thomas, a clinical teacher for the Welsh National School of Medicine, conceived the idea of a donor system for corneal grafts and an eye bank was established in East Grinstead in 1955.
These are organizations located throughout the world to coordinate the distribution of donated corneas to surgeons, as well as providing eyes for research.
Since 2004, Amnitrans Eyebank in Rotterdam, The Netherlands, provides donor corneas pre-cut for advanced keratoplasty procedures, such as DSEK, DSAEK, FS-DSEK and DMEK.
An upcoming systematic review will seek to compare the safety and effectiveness of DMEK versus DSAEK in people with corneal failure from Fuchs' endothelial dystrophy and pseudophakic bullous keratopathy.
This technique, which proved successful in mouse trials, would be of use to those with inherited genetic degenerative conditions of the cornea, especially if other means like a transplant are not feasible.
On 25 August 2010, investigators from Canada and Sweden reported results from the first 10 people in the world treated with the biosynthetic corneas.
To make the material, the researchers placed a human gene that regulates the natural production of collagen into specially programmed yeast cells.
[38] A 2013 cost-benefit analysis by the Lewin Group for Eye Bank Association of America, estimated an average cost of $16,500 for each corneal transplant.