Bariatric surgery
[12] Stomach reduction surgery is frequently used for cases where traditional weight loss approaches, consisting of diet and physical activity, have proven insufficient, or when obesity already significantly affects well-being and general health.
[12] Similarly, the American Academy of Pediatrics recommends bariatric surgery for adolescents 13 and older with a BMI greater than 120% of the 95th percentile for age and sex.
[15] As of October 2024,[update] there has been a reported 30% drop in bariatric surgeries in the United States during the past year, and this can be attributed to GLP-1s such as Novo Nordisk's Ozempic and Wegovy.
[12] In the three decades that followed, obesity rates continued to rise, laparoscopic surgical techniques made the procedure safer, and high-quality research showed effectiveness at improving health among various conditions.
[20] As of 2019,[update] the American Academy of Pediatrics recommended bariatric surgery without age-based eligibility limits under the following indications: BMI more than 35 with severe comorbidity, such as obstructive sleep apnea (Apnea-Hypopnea Index above 0.5), type 2 diabetes, idiopathic intracranial hypertension, nonalcoholic steatohepatitis, Blount disease, slipped capital femoral epiphysis, gastroesophageal reflux disease, and idiopathic hypertension or a BMI above 40 without comorbidities.
[21] Surgery is contraindicated with a medically correctable cause of obesity, substance abuse, concurrent or planned pregnancy, eating disorder, or inability to adhere to postoperative recommendations and mandatory lifestyle changes.
[30][29] No significant difference was noted for changes in cholesterol, or LDL, but HDL did increase in the surgical groups, and reduction in blood pressure was variable between studies.
[31] While weight loss is essential in T2DM management, sustaining improvements long-term is challenging; 50% to 90% of people struggle to achieve adequate diabetes control, suggesting the need for alternative interventions.
[32][33] In this context, studies have reported an 85.3–90% resolution of T2DM after bariatric surgery, measured by reductions in fasting plasma glucose and HbA1C levels, and remission rates of up to 74% two years post-surgery.
[33][30][32] The International Diabetes Federation Task recommends bariatric surgery under certain circumstances, including failure of conventional weight and T2DM therapy in individuals with a BMI of 30–35.
Notably, chronic vitamin D deficiency may contribute to osteoporosis; insufficiency fractures, especially of the upper extremity, are of higher incidence in bariatric surgery patients.
[45] An early complication of Roux-En-Y Gastric Bypass: Small bowel obstruction, which can be caused by the internal hernias due to the laparoscopic RYGB surgery techniques that were used.
[48] Late dumping syndrome is characterized by low blood sugar 1–3 hours after a meal, presenting with palpitations, tremors, sweating, a feeling of faintness, and irritability.
Infant mortality, preterm birth, small fetal size, congenital anomalies, and NICU admission are all elevated in bariatric surgery patients.
[2][4] For instance, while sleeve gastrectomy (discussed below) was initially thought to work simply by reducing the size of the stomach, research has begun to elucidate changes in gut hormone signaling as well.
[18] Studies have shown that bariatric procedures may have additional effects on the hormones that affect hunger and satiety (such as ghrelin and leptin), despite initial development to target reduction of food intake and/or nutrient absorption.
[18] The risk of ulcers or narrowing of the gut due to intestinal strictures is less so with sleeve gastrectomy versus Roux-en-Y gastric bypass, but it is not as effective at treating GERD or type 2 diabetes.
[2][4] Though initially thought to work strictly by reducing the size of the stomach, recent research has shown that there are also changes in gut signaling hormones with this procedure leading to weight loss.
[2][56] The sleeve gastrectomy mechanism works by creating a narrow gastric lumen which restricts food intake and prevents receptive relaxation, alongside ongoing research into hormonal changes, and gastrointestinal motility.
[57][58] The physical mechanism that will make the SG stand out to other bariatric surgery is its reduction of the storage of the stomach significantly, allowing patients to control their calorie intakes.
Changes in the gut microbial community post-SG may influence energy harvest from the diet, impact inflammatory pathways, and affect the host's metabolic profile.
[57] Techniques: After 1-3 postoperative days, patients begin oral intake, contingent on a successful gastrografin leak test, and receive continuous metabolic monitoring.
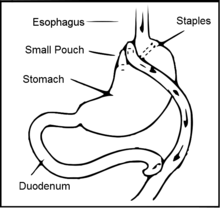
[60] Roux-en-Y gastric bypass surgery involves the creation of a new connection in the gastrointestinal tract, from a smaller portion of the stomach to the middle of the small intestine.
[18] A 2021 evidence update comparing the benefits and harms of bariatric procedures found that Roux-en-Y gastric bypass surgery and sleeve gastrectomy both effectively reduced weight and led to Type 2 diabetes remission.
[64] Weight loss following the surgery is largely due to the alteration of gut hormones that control hunger and satiety, as well as the physical restriction of the stomach and decrease in nutrient absorption.
[72] This procedure where a device similar to a heart pacemaker that is implanted by a surgeon, with the electrical leads stimulating the external surface of the stomach, was under preliminary research in 2015.
[73] Electrical stimulation is thought to modify the activity of the enteric nervous system of the stomach, which is interpreted by the brain to give a sense of satiety, or fullness.
In general, immediately after bariatric surgery, the person is restricted to a clear liquid diet, which includes foods such as broth, diluted fruit juices, or sugar-free drinks.
[74] Bariatric plastic surgery procedures, sometimes called body contouring, may be an option for people wishing to remove excess skin following the large change in weight.
[83] Difficulties surrounding obesity treatment selection among children and adolescents include ethical considerations when obtaining consent from those who may be unable to do so without adult guidance or understanding the potential lasting effects of invasive procedures.