Monoamine transporter
Furthermore, drugs such as MDMA[3] ("ecstasy", "molly") and natural alkaloids such as cocaine exert their effects in part by their interaction with MATs, by blocking the transporters from mopping up dopamine, serotonin, and other neurotransmitters from the synapse.
[2] DATs can be found in the central nervous system (CNS), where they are localized in the substantia nigra and ventral tegmental area (VTA).
[2] In the CNS, SERT is found localized in the cerebral cortex, CA1 and CA3 regions of the hippocampus, as well as the median and dorsal raphe nuclei.
Regulation of SERT has been linked to acute depletion of intracellular Ca Na 2+, calmodulin inhibition, CaMKII, Src, p38 MAP kinase, PKC, and activation of NOS/cGMP.
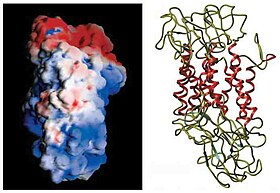
[5] MATs are large integral membrane proteins composed of 12 transmembrane domains connected by intracellular and extracellular loops.
The ion concentration gradient generated by the plasma membrane Na+/K+ ATPase provides the driving force for the transporter-mediated monoamine uptake.
Evidence supporting this belief includes that monoamine transporters, DAT, NET, and SERT, are important target sites for therapeutic drugs used in the treatment of mood disorders.
Methylphenidate (Ritalin) inhibits both DAT and NET, which results in an increase in extracellular dopamine and norepinephrine that can readily bind postsynaptic cells.
Selective serotonin reuptake inhibitors (SSRIs) are the most widely used antidepressant and include fluoxetine (Prozac), citalopram (Celexa), and fluvoxamine (Luvox).
These chemicals inhibit the action of DAT and, to a lesser extent, the other monoamine transporters, but their effects are mediated by separate mechanisms.
Monoamine transporters are established targets for many pharmacological agents that affect brain function, including the psychostimulants cocaine and amphetamine.
Axelrod eventually received his Nobel Prize for this research, which led to the discovery of DATs and SERTs as well as consequences associated with antidepressant and psychostimulant interactions with MAT proteins.
Since Axelrod's initial studies, understanding the pharmacological and functional properties of MAT proteins have been essential in the discovery of therapeutic treatment of many mental disorders.
In 1991 Susan Amara and her colleagues determined the amino acid sequence of NET, discovering its relatively high coding similarities to that of the GABA transporter.
[1][13] Over the last decade, the availability of targeted disruption of monoamine transporter genes in animal models as well as in vivo imaging approaches have shown progress in studies associated with psychiatric and movement disorders.
[1] Ongoing research is attempting to clarify the extent to which kinase cascades, transporter interacting proteins, and phosphorylation contribute to MAT regulation.
SSRI's such as Fluoxetine (Prozac) and SNRI's as with Venlafaxine are the main types of drugs given in first line depression and anxiety treatment.