Mouth ulcer
The two most common causes of oral ulceration are local trauma (e.g. rubbing from a sharp edge on a broken filling or braces, biting one's lip, etc.)
and aphthous stomatitis ("canker sores"), a condition characterized by the recurrent formation of oral ulcers for largely unknown reasons.
This type of lesion is tangential to the rete pegs and shows punctiform (small pinhead spots) bleeding, caused by exposed capillary loops.
[10] The vesicles and bullae of blistering mucocutaneous disorders progress quickly to ulceration in the mouth, because of moisture and trauma from food and teeth.
However, the epithelia of the mouth also has a high turnover rate and makes oral ulceration (mucositis) a common side effect of chemotherapy.
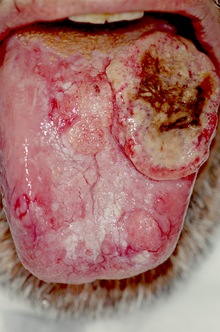
When the full thickness of the epithelium is penetrated (ulceration), the lesion becomes covered with a fibrinous exudate and takes on a yellow-grey color.
Repeat episodes of mouth ulcers can be indicative of an immunodeficiency, signaling low levels of immunoglobulin in the oral mucous membranes.
The following details may be pertinent: The duration that the lesion has been present, the location, the number of ulcers, the size, the color and whether it is hard to touch, bleeds or has a rolled edge.
A biopsy (minor procedure to cut out a small sample of the ulcer to look at under a microscope) with or without immunofluorescence may be required, to rule out cancer, but also if a systemic disease is suspected.
), vesicles and bullae which form on the mucous membranes of the oral cavity tend to be fragile and quickly break down to leave ulcers.
The mucous membrane lining of the mouth is thinner than the skin, and easily damaged by mechanical, thermal (heat/cold), chemical, or electrical means, or by irradiation.
[citation needed] Common causes of oral ulceration include rubbing on sharp edges of teeth, fillings, crowns, false teeth (dentures), or braces (orthodontic appliances), or accidental biting caused by a lack of awareness of painful stimuli in the mouth (e.g., following local anesthetic used during dental treatment, which the person becomes aware of as the anesthetic wears off).
Some people cause damage inside their mouths themselves, either through an absentminded habit or as a type of deliberate self-harm (factitious ulceration).
[citation needed] The lingual frenum is also vulnerable to ulceration by repeated friction during oral sexual activity ("cunnilingus tongue").
Microwave ovens sometimes produce food that is cold externally and very hot internally, and this has led to a rise in the frequency of intra-oral thermal burns.
Thermal food burns are usually on the palate or posterior buccal mucosa, and appear as zones of erythema and ulceration with necrotic epithelium peripherally.
[14][16] Caustic chemicals may cause ulceration of the oral mucosa if they are of strong-enough concentration and in contact for a sufficient length of time.
Holding an aspirin tablet next to a painful tooth in an attempt to relieve pulpitis (toothache) is common, and leads to epithelial necrosis.
Silver nitrate, sometimes used for pain relief from aphthous ulceration, acts as a chemical cauterant and destroys nerve endings, but the mucosal damage is increased.
This usually occurs in the mandible, and causes chronic pain and surface ulceration, sometimes resulting in non-healing bone being exposed through a soft tissue defect.
Other possible causes include hematinic deficiency (folate, vitamin B, iron), stopping smoking, stress, menstruation, trauma, food allergies or hypersensitivity to sodium lauryl sulphate (found in many brands of toothpaste).
Aphthous stomatitis has no clinically detectable signs or symptoms outside the mouth, but the recurrent ulceration can cause much discomfort to those affected.
[citation needed] Opportunistic activity by combinations of otherwise normal bacterial flora, such as aerobic streptococci, Neisseria, Actinomyces, spirochetes, and Bacteroides species can prolong the ulcerative process.
Fungal causes include Coccidioides immitis (valley fever), Cryptococcus neoformans (cryptococcosis), and Blastomyces dermatitidis ("North American Blastomycosis").
Malignant lesions also typically feel indurated (hardened) and attached to adjacent structures, with "rolled" margins or a punched out appearance and bleeds easily on gentle manipulation.
[21] If someone has an unexplained mouth ulcer persisting for more than 3 weeks this may indicate a need for a referral from the GDP or GP to hospital to exclude oral cancer.
If individuals allergic to this substance have oral exposure they may experience stomatitis and cheilitis (inflammation, rash, or painful erosion of the lips, oropharyngeal mucosa, or angles of their mouth).
[24][25][26][27] Balsam of Peru is used in foods and drinks for flavoring, in perfumes and toiletries for fragrance, and in medicine and pharmaceutical items for healing properties.
Dermatological causes include chronic ulcerative stomatitis, erythema multiforme (Stevens-Johnson syndrome), angina bullosa haemorrhagica and lichen planus.
Other examples of systemic disease capable of causing mouth ulcers include lupus erythematosus, Sweet syndrome, reactive arthritis, Behçet syndrome, granulomatosis with polyangiitis, periarteritis nodosa, giant cell arteritis, diabetes, glucagonoma, sarcoidosis and periodic fever, aphthous stomatitis, pharyngitis and adenitis.