Neuropsychopharmacology
The first half of the 20th century saw psychology and psychiatry as largely phenomenological, in that behaviors or themes which were observed in patients could often be correlated to a limited variety of factors such as childhood experience, inherited tendencies, or injury to specific brain areas.
Indeed, the behavioral branch of psychology dispensed altogether with what actually happened inside the brain, regarding most mental dysfunction as what could be dubbed as "software" errors.
In the same era, the nervous system was progressively being studied at the microscopic and chemical level, but there was virtually no mutual benefit with clinical fields—until several developments after World War II began to bring them together.
Neuropsychopharmacology may be regarded to have begun in the earlier 1950s with the discovery of drugs such as MAO inhibitors, tricyclic antidepressants, thorazine and lithium which showed some clinical specificity for mental illnesses such as depression and schizophrenia.
The prominent methods which could directly affect brain circuitry and neurotransmitter levels were the prefrontal lobotomy, and electroconvulsive therapy, the latter of which was conducted without muscle relaxants and both of which often caused the patient great physical and psychological injury.
More profoundly, though, the knowledge gained may provide insight into the very nature of human thought, mental abilities like learning and memory, and perhaps consciousness itself.
A direct product of neuropsychopharmacological research is the knowledge base required to develop drugs which act on very specific receptors within a neurotransmitter system.
For example, contrary to previous thought, it is now known that the adult brain does to some extent grow new neurons—the study of which, in addition to neurotrophic factors, may hold hope for neurodegenerative diseases like Alzheimer's, Parkinson's, ALS, and types of chorea.
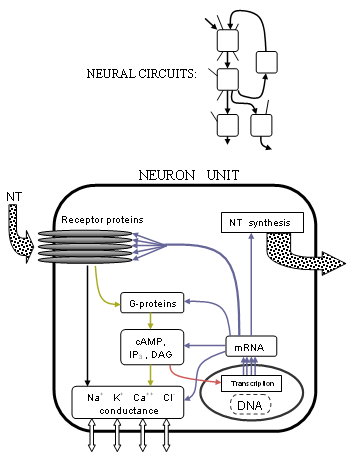
In this way signals are generated and carried through networks of neurons, the bulk electrical effect of which can be measured directly on the scalp by an EEG device.
[4] These features are: The more recent advances involve understanding at the organic molecular level; biochemical action of the endogenous ligands, enzymes, receptor proteins, etc.
The concentration differences between the inside and outside of the cell determine the membrane voltage.Precisely how these currents are controlled has become much clearer with the advances in receptor structure and G-protein coupled processes.
The FDA has approved drugs which selectively act on each of the major neurotransmitters such as NE reuptake inhibitor antidepressants, DA blocker anti-psychotics, and GABA agonist tranquilizers (benzodiazepines).
The next step, which major pharmaceutical companies are currently working hard to develop, are receptor subtype-specific drugs and other specific agents.
Modern studies are revealing details of mechanisms of damage to the nervous system such as apoptosis (programmed cell death) and free-radical disruption.
As for MDMA, aside from persistent losses of 5HT and SERT, long-lasting reduction of serotonergic axons and terminals is found from short-term use, and regrowth may be of compromised function.
Functional associations of brain anatomy are now being complemented with clinical, behavioral, and genetic correlates of receptor action, completing the knowledge of neural signalling (see also: Human Cognome Project).
This can lead the individual to engage in mild to extreme drug-seeking behaviors as the brain begins to regularly expect the increased presence of dopamine and the accompanying feelings of euphoria, but how problematic this is depends highly on the drug and the situation.
It is at this point known with relative certainty that the primary shared effects of a broad pharmacological group of hallucinogens, sometimes called the "classical psychedelics", can be attributed largely to agonism of serotonin receptors.
One hypothesis suggests that in the frontal cortex, 5HT2A promotes late asynchronous excitatory postsynaptic potentials, a process antagonized by serotonin itself through 5HT1 receptors, which may explain why SSRIs and other serotonin-affecting drugs do not normally cause a patient to hallucinate.
GABAergic neurons from the SCN inhibit the paraventricular nucleus, which signals the superior cervical ganglion (SCG) through sympathetic fibers.
The output of the SCG, stimulates NE receptors (β) in the pineal gland which produces N-acetyltransferase, causing production of melatonin from serotonin.
Additionally, (not shown in diagram), the basal nucleus provides GABA-ergic inhibitory input to the pre-optic anterior hypothalamus (PAH).
For example, the addictive stimulant drug cocaine has long been known to act upon the reward system in the brain, increasing dopamine and norepinephrine levels and inducing euphoria for a short time.
[9] These findings are important because they provide detailed insight into the neural circuitry involved in drug use and help refine old as well as develop new treatment methods for disorders or addictions.
Different treatment-related studies are investigating the potential role of peptide nucleic acids in treating Parkinson's disease and schizophrenia[10] while still others are attempting to establish previously unknown neural correlates underlying certain phenomena.
It is one measure of the state of knowledge in 2002, and might be said to represent a landmark in the century-long goal to establish the basic neurobiological principles which govern the actions of the brain.